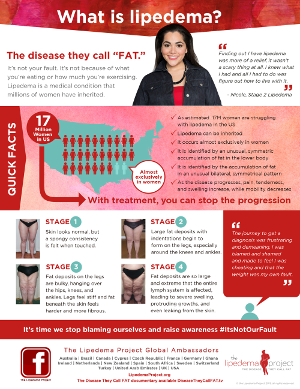
What is Lipedema
Lipedema was first formally identified in the U.S. at the Mayo Clinic in 1940 (1). However, not much research and diagnosis criteria have been established to battle this adipose connective tissue disorder for more than 75 years. It has only been within the last 10 years we have seen a surge in people, mostly women, presenting with symptoms looking for a diagnosis and treatment plan.
There is no known cure for Lipedema. Physicians are not readily trained to diagnose Lipedema from Lymphedema and general obesity. More training and education is needed in the area of adipose tissue and lymphatic disorders to facilitate patients into proper treatment! Lipedema Simplified has created a Physician’s Training Guide to help clinicians identify and diagnosis those with suspected Lipedema.
Let’s learn more about what is Lipedema.
Defining Lipedema
Lipedema (or Lipoedema as it is spelled in the European community) is a progressive chronic disease of fat tissue that affects more than 11 percent woman and less than 1 percent of men worldwide. This adipose connective tissue disorder is characterized by bilateral symmetrical swelling of the legs, thighs and hips. The hips and thighs usually start enlarging disproportionately to the rest of the body thus giving you a pear shaped body appearance. We are also starting to see more Lipedema patients with enlarged upper arms that display the classic lipomas in the lower section too. Clinicians and patients commonly confuse Lipedema with general obesity, which classically has an apple shaped body appearance.
Lipedema is often called the “painful fat syndrome” as abnormal fat cells cluster together and expand under the skin. Interstitial fluid increases between the clusters creating pain to touch or when standing. People in the later stages often complain about pain when being touched or even walking where pockets of fat press on nerves.
They may also easily bruise either from bumping into objects or overstretching your limb when capillaries embedded in the fat cluster burst. Bruising may also take longer to heal in Lipedema patients.
For those with Lipedema in the upper arms care needs to be observed when taking blood pressure. Patients should NEVER have their blood pressure taken in the upper arm as it can induce severe pain and bruising. Tell your clinician to take your blood pressure in your lower arm only! Even then you may experience pain and bruising if you have lipomas under the skin.
Cause of Lipedema
The cause of Lipedema is unknown at this point. There are no identified genetics markers, blood tests or imaging scans yet that can pinpoint Lipedema. There is observable evidence of Lipedema being present in mother and biological daughter(s) meaning there is a possible hereditary component. In my case, Lipedema, Lymphedema and Dercum’s Disease was present in my paternal grandmother so it may also be possible men may carry genetic markers for the condition which is then passed on to a biological daughter(s).

Lipedema researchers are also investigating whether metabolism, inflammation and hormonal changes are responsible for the development of the disease. Unfortunately, there are no tests available to diagnose the condition; it is purely based on palpable observation and symptomology. Whatever the etiology of this disease it is still not readily recognized by the medical community with many women being undiagnosed for years!
Many women report the most significant changes in adipose fat occur during life changes, such as puberty, childbirth, surgery and menopause when hormones are fluctuating. Mothers should pay careful attention to their daughters during and following puberty for any abnormal fat development or pain when touching the skin. It is imperative that women be vigilant about changes to their bodies, particularly the hips, thighs, lower legs and upper arms after a physical life change so that early diagnosis and treatment can begin.
A recent 2024 paper on an “Observational Study on a Large Italian Population with Lipedema: Biochemical and Hormonal Profile, Anatomical and Clinical Evaluation, Self-Reported History” has provided further insight into the symptomology and evolution of Lipedema.
Immune to Diet and Exercise
Lipedema does not discriminate on body size, shape or ethnicity. Women who are thin or obese are equally at risk of developing this disease. It is however, a predominately female-based disease. Some are surmising it is mostly confined to genetics of the X chromosome, with less than one percent of Lipedema occurring in men.
This fat disease is also resistant to diet and exercise. Nearly all women have tried numerous dieting and exercising plans in an effort to drop the excess weight in their hips, thighs and legs to no avail, myself included. Some have noticed some weight loss but is was usually in places not affected by Lipedema, such as in the torso. Can you imagine the frustration in expending all that time, energy and money to try and lose weight only to learn this disease is resistant to diet and exercise!
Try to imagine the pain and shame of a body-bias culture where being larger than the accepted “normal” figure elicits frustration and disgust. Trying to hide large or even disfigured limbs is exhausting and expensive as larger or custom-made garments are necessary to fit a disproportionate body frame. For many, these types of prevalent body-bias and impaired mobility from the disease have forced many women into social isolation.
This body-bias even happens by medical professionals who perpetuate the “diet and exercise more” scenario. solely based on physical presentation. There are conditions beyond obesity that produce similar body types that simply do not respond well to diet and exercise. There needs to be an increased awareness of Lipedema within the medical community so patients can get the validation and treatment necessary to managing this disease! Nothing hurts more than a summary dismissal of the possibility of a fat disease and a lack of true weight loss effort on the patient’s part! This can be so demeaning and frustrating for women searching for answers to feel blamed and shamed for something that it out of their control!
What patients need to hear after diagnosis is: LIPEDEMA IS NOT YOUR FAULT!! It is an incurable disease that requires ongoing maintenance to yield the best quality of life possible. Let’s keep the advocacy and education work going so patients get the proper diagnosis, emotional, social, and mental support, and medical resources required to treat this disease.
Patients can advocate for themselves using Lipedema Foundation’s Self Advocacy Guide.
Clinician’s and patients should review the most recent (2021) Standard of Care for Lipedema for the US for guidance.
Lipedema Phenotypes
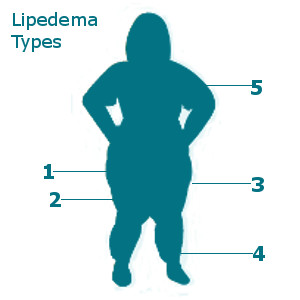
Lipedema can affect one or more areas of the body in people with the disease. Because not all people present with the same exact affected areas it takes a clinician skilled in adipose tissue disorders to diagnose it properly, especially when the disease is in its early stages.
Type 1 – Buttocks: excess buildup of fat in the buttock area disproportionate to other body areas. Can cause discomfort when sitting and moving around.
Type 2 – Buttock, Hip and Thigh: excess buildup of fat in buttock, thigh and thigh area with swelling causing pain and discomfort. More common than Type 1.
Type 3 – Buttock, Hip, Thigh and Calves: excess buildup of fat in the entire lower body area with swelling causing pain and discomfort. Most common type of Lipedema.
Type 4 – Calves: (or “cankles”) less common only calves are involved. Swelling in ankles causing pain and possible mobility issues.
Type 5 – Upper Arms: least common type of Lipedema. Heaviness and swelling in the upper arms cause discomfort. Can present with any of the other types of Lipedema.
Can you identify what areas of your body are affected by Lipedema? In addition to body types there are progressive stages of Lipedema.
Stages of Lipedema
Lipedema is a progressive fat disease meaning if no treatment is applied fat cells are likely to increase in size and cluster, As the disease progresses the hips, thighs, lower legs and sometimes the upper arms will increase in size and pain. The skin texture will change from spongy fat to a dimpling effect as fat cells create bulging in the hips, thighs and legs. Eventually the lymphatic and vascular systems become compromised causing excessive painful swelling, excess skin pockets that fold over the legs, knees and ankles and severe lymphedema.
Recognizing the stages of Lipedema is critical to getting a diagnosis and a treatment plan to avoid progression to the next stage. There are four stages of this disease:
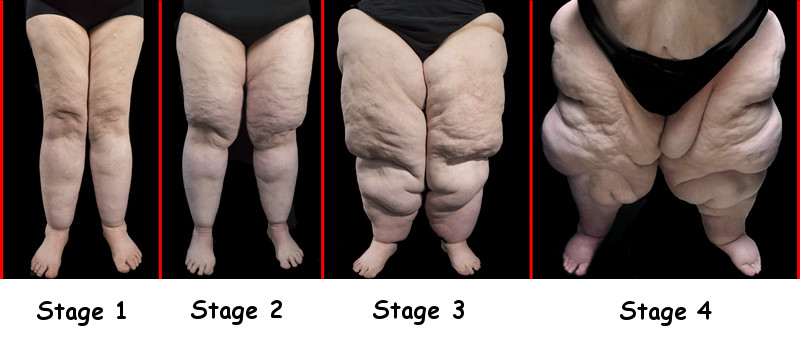
Stage 1
This stage is probably the most difficult to diagnose as it may appear like normal weight gain. This is where you need to be evaluated by someone trained in fat disorders or who can distinguish the difference between normal fat and Lipedema fat.
Here are the most common symptoms:
- Excess fat in legs that looks disproportionate to the upper body. Weight loss does not affect the lower body area. The look and feel of fat is symmetrical and evenly distributed from the hips to the ankles. Padding around knees can make it harder to differentiate normal from Lipedema fat.
- Skin is generally smooth, healthy in color and not discolored. May feel spongy to the touch.
- No excess fat in ankles or feet.
- Pain may be present with or without pressure.
- Fat deposit may feel lumpy and be dispersed among affected area, like peas or marbles.
- May bruise more readily in affected area
- Stemmer’s sign is negative (when you pinch the skin near the toes you can lift the skin off the foot).
- No pitting of the skin (pressing in the skin with your thumb does not leave an indent that slowly fills and disappears).
- May have swelling in the ankles or feet that disappear when legs are elevated.
- Responds well to treatment.
Stage 2
When left undiagnosed and untreated Lipedema will progress to the next level.
Here are the most common symptoms:
- All of the stage 1 symptoms
- Skin starts to show indentations
- Lipomas may develop (large fat clusters ranging from pea size to fist size located between the skin and muscle layers)
- Dry itching skin or Eczema in patches across the Lipedema areas
- Swelling of the legs, especially lower legs, that when elevated does not bring much relief or reduction
- Should respond well to treatment
Stage 3
Unlike Stage 1 and Stage 2 progression, which may happen in a short period of time, Stage 3 may take several years to develop.
Here are the most common symptoms:
- Excess skin and fat in the thighs and legs continue to grow in size and eventually create skin folds and creases (also known as saddlebags, shelves or cuffs) that overhang knees and ankles.
- Skin is largely bumpy in look and touch.
- Hardened connective fibrotic tissue is present (from stagnation of fluid and protein movement)
- No excess fat in ankles or feet.
- Lipomas may increase in number and size and are painful with or without touch.
- Appearance of varicose and spider veins
- May present with Livedo reticularis, which is a netlike mesh pattern of capillaries showing just under the skin
- Bruising happens more readily in affected areas.
- Lower legs, feet and toes may feel colder than the rest of the body (a form of hypothermia)
- Stemmer’s sign is still negative.
- Pitting of the skin is present.
- Swelling is consistently present and will not be relieved by leg elevation or sleeping.
- Mobility and gait issues may occur from the location of excess fat interfering with normal daily activities.
- Treatment is less responsive in this stage
Stage 4
Unlike Stage 1, 2 and 3 progression, Stage 4 may take several more years to develop. This stage incorporates a secondary condition called Lymphedema, which is caused by severe Lipedema fat deposits blocking key areas of the lymphatic system. Even though the lymph system tries to create new pathways there is too much fluid and protein retention to adequately move out the legs, thighs and hips causing extreme swelling. This stage is also known as Lipo-Lymphedema.
While Lipo-Lymphedema is the most common type of Lipedema at this stage someone may also present with Lipo-Phlebolymphedema, which includes the symptoms per stage below, and a reddish or purplish discoloration in the lower legs between the calves and the ankles. This discoloration, or hyperpigmentation, is a sign of chronic venous insufficiency (CVI) where inflammation of the subcutaneous fat causes blood to pool in the affected area. If left untreated someone may be looking at the further development of lipodermatosclerosis, which is the hardening of the affected skin area.
Here are the most common symptoms:
- Excess skin and fat in the thighs and legs continue to grow in size, eventually create skin folds and creases that overhang knees and ankles.
- Skin increases in its bumpy look and touch. May also present with hyperkeratosis or thickening of the outer layer of skin.
- Additional massive localized lymphedema lobules may appear on the back of the leg(s) or inner thighs making walking difficult to impossible (immobility). Legs are no longer symmetrical and could present as elephantiasis.
- Hardened connective fibrotic tissue is present in multiple areas.
- Some may have excess swelling in feet. (Stemmer’s sign is positive.)
- Appearance of varicose and spider veins
- May present with Livedo reticularis, which is a netlike mesh pattern of capillaries showing just under the skin
- Lower legs, feet and toes may feel colder than the rest of the body (a form of hypothermia)
- Lipomas may increase in number and size with increased pain regardless of touch or not.
- Venous Insufficiency (inability to maintain good blood supply through the affected area) may occur causing skin dermatitis or varicose veins.
- Lipedema may spread to both upper arms causing significant swelling and pain from lipomas.
- Lipedema may spread to abdomen causing creation of large panis (belly that hangs down past private areas) and may be painful from lipomas. (Causes problems with mobility and gait.)
- Increased occurrence of sores and tears in the skin from cellulitis infection and poor hygiene.
- Increased bruising happens more readily in affected areas.
- Pressure ulcers may develop if immobile or sitting/lying down too long
- Pitting of the skin is present.
- Swelling is consistently present and will not be relieved by leg elevation or sleeping.
- Treatment is difficult. Need to treat for Lymphedema (covered in separate section).
Here is a video from the Lipedema Project demonstrating a mother and daughter with Lipedema:
Anyone experience additional signs of Lipedema in the various stages? Can you identify where you might fall in the various stages of Lipedema? I am definitely Stage 4 and have been for many years. It can be disfiguring and very challenging to walk. My prayer would be for anyone with Lipedema to be diagnosed early and get treatment so that progression can be halted in Stage 1 or 2 without all the debilitating problems that come in Stage 3 and 4!
Check out our next section on diagnosing Lipedema.
To your improved health!
References:
(1) – Allen E V, Hines E A, Lipoedema of the legs. A syndrome characterized by fat legs and edema. Proc Staff. Meet. Mayo Clinic 1940; 15:184
Resources:
- Lipedema Foundation – Resources for Learning More
- Sage Journals – Standard of Care for Lipedema in the United States
- Lipedema.com – Other Countries Lipedema Standards of Care
- Fat Disorders Resource Society – Fat Disorders Resource Society