Skin and Wound Care
Wounds are the enemies of those suffering with adipose tissue and lymphatic diseases, especially those with Lymphedema and Lipo-Lymphedema! Some wounds causing minor symptoms like redness or itchy and other wounds can outright kill you. It is essential to learn about skin and wound care when you have Lipedema and Lipo-Lymphedema. When you have one of these diseases you need to be constantly vigilant about items around you that can cause you harm, such as:
- items that can cut, scrape, puncture or bruise – furniture, open drawers, items with sharp edges, plants
- animals in your care – claw scratches or teeth bites
- items that can burn you – hot stove, oils, fireplaces, fire pits, heaters
- animals that sting – mosquitoes, bees, reptiles
- hidden items that make you sick – germs, strong fumes, others with unclean body parts or contagious conditions
These kinds of situations can cause injury to your already damaged limb(s), arm(s), neck, face or abdomen areas. One minute of injury can cause hours, days, weeks or months of great discomfort, relentless itching, burning skin, weeping, and agonizing pain that may require professional assistance from emergency room staff, your doctor or a wound care clinic. It is important to reduce your exposure to those things that cause you harm and to know what to do once you have sustained an injury. Here is a common list of wounds and what you can do to mitigate them.
Bruising
Most people will dismiss a small patch of black and blue as nothing to worry about. However, for those with impaired lymphatics or fat disorders need to understand that bruising is something to monitor for excessive bleeding under the skin and if the skin breaks.
 Bruises that result in skin breaks need to evaluated if a doctor’s attention is required. Skin breaks that bleed help clean out the wound. Do not use iodine or hydrogen peroxide, which are toxic to cells of wound, to clean out the wound. Use an antibacterial soap and water to gently clean the wound. You can use neosporin if you can tolerate it (some are allergic) or just dress the wound with suitable size bandage or gauze pad with (allergen free) medical tape. Monitor for proper healing.
Bruises that result in skin breaks need to evaluated if a doctor’s attention is required. Skin breaks that bleed help clean out the wound. Do not use iodine or hydrogen peroxide, which are toxic to cells of wound, to clean out the wound. Use an antibacterial soap and water to gently clean the wound. You can use neosporin if you can tolerate it (some are allergic) or just dress the wound with suitable size bandage or gauze pad with (allergen free) medical tape. Monitor for proper healing.
Bruises without broken skin that are large in size should be treated with ice for 20 minutes to help reduce the swelling around the affected area. You can also alternate ice and heat on the bruised area for 24 hours. Bruising will cause additional swelling in an area that is already swollen with excess lymph fluid. To facilitate reduction in swelling you can perform a self massage on the area around the bruise to manually move fluid. Gently move your hand along the skin towards the direction of the heart. Then massage the areas of your trunk to keep fluid moving towards the heart. Major node clusters are located in your groin, your neck and your armpits.
Personal: I just recently healed a large bruise about eight inches in diameter in the skin fold above my right knee that happened when overstretching to the knee burst a blood vessel in my Lipedema fat. It was painful and swelled up large enough to put pressure on the knee area. I used ice and manual massage to move the excess fluid out out the area. It took about five weeks to completely heal the area.
Minor Cuts, Punctures and Scrapes

Anything that breaks the skin in an area with Lymphedema can be complicated. Some cuts or puncture may only weep (slow leak) lymph fluid, also known as lymphorrhea, , some may bleed and some may do both. Skin breaks that bleed help clean out the wound. Do not use iodine or hydrogen peroxide to clean out the wound. Use an antibacterial soap and water to gently clean the wound. You can use neosporin if you can tolerate it (some are allergic) or just dress the wound with suitable size bandage or gauze pad with (allergen free) medical tape. Elevate the affected area to help get excess fluid moving away from the wound.
Don’t panic if a clean weeping cut or puncture doesn’t heal for a day or two. Bleeding should stop fairly quickly. If after cleaning the area, elevation and bandaging still doesn’t work you will want to contact your doctor or emergency room for assistance. You need to be vigilant with ANY open wound that you do not contract a bacterial infection!
Personal: most of puncture happen from my dog or cat’s nails. Most of them will weep for a couple hours to a day before closing the hole. I make sure to clean all scrapes and punctures to avoid infection. I have had one major infection that I do not wish to repeat!
Rashes

Rashes can be caused by outside factors, such as poison ivy, sumac, oak, by other plants, or by something applied topical or ingested. It can also manifest by internal reactions caused by an overaction of mast cells, such as in those who have one of the Mast Cell Diseases (MCD), particularly MCAS (mast cell activation syndrome). Rashes caused by any of the MCD need to be watched closely for any signs of anaphylaxis, which can become life threatening.
The rash may be a small patch, encase a good part of a limb or be systemic. It can also present with fluid-filled blisters or large hives. DO NOT ITCH the affected area! I know that is hard to do, but you need to remember opening any portal in your skin will invite unwanted bacteria infections.
If you can tolerate topical cortisone creams you can use one on your rash area to help quell itching and quiet the affected area. If you have never used a cortisone cream or the over the counter cream isn’t working consult your doctor for something you can tolerate. Keep the area clean and call your doctor if anything changes in the look and feel of the rash.
Personal: I have also used good old Calamine lotion and cold wet washcloths to help with the itching. Boy, was it hard not to itch the area. I also had a whole body hive with raised welts situation due to an allergic reaction to ibuprofen. I used topical cream, cold washcloths, Calamine lotion and Benadryl (at the advice of my doctor) to help combat the hives, which took two weeks to clear up.
Burns
Burns on lymphedema skin require special care and attention which includes consulting your doctor or emergency room. Do NOT place butter, oil, ice, or ice water on burns!
-
1st, 2nd and 3rd degree burns 1st degree burns are known as superficial burns. There are no breaks in the skin or blisters. You can treat these burns by holding the affected area under cool running water or using a cold wet washcloth for 20 minutes. After that you can an antibiotic cream or low pH moisturizer to treat the area. You can also use a light bandage to help protect the burn area.
- 2nd degree burns have blisters and damage to the outer layer of skin. This constitutes a break in the lymphedema skin and should be treated immediately by your doctor or emergency room department.
- 3rd degree burns are the most severe and require immediate attention by emergency room physicians. These burns destroy all layers of the skin, the underlying fat, muscles, bones and nerves. These burns can be life threatening especially those with compromised systems, such as those with Lymphedema.
Skin Tears and Fungal Infections

In advanced stages of Lymphedema or Lipo-Lymphedema you will have folds of skin that may overhang the knees, ankles, upper thighs and belly (called a panis). Inside these folds are skin creases that are thin and hidden from circulating air. This creates a perfect stage for fungal or yeast infections to develop and thrive. If not cleaned regularly the hot moist climate will cause the skin to weaken and either an infection or skin tear may occur. This makes moving painful as the affected areas rub together.
For fungal infections I recommend cleaning the area very well and applying an anti-fungal cream that blocks their growth and keeps the are dry. You can use it under your belly/panis, under your breasts or even on your backside (if you have trouble keeping yourself sparkling clean).
For skin tears you need to clean the area well and apply a topical antibiotic (sometimes over the counter Neosporin will work or you may need something stronger in prescription form) to help seal and heal the tear. Keep reapplying as necessary until the tear has healed.
Personal: I had a skin tear in my upper left thigh area that may sleeping very painful as I can only sleep on my left side. Neosporin didn’t works this time but the prescription antibiotic topical cream did. It took four to seven days to heal and I had to sleep with a pillow between my legs to avoid it rubbing with the other leg. Walking was also somewhat painful.
Bacterial Infections
Bacterial infections in the affected lymphedema limb are the most frequent and serious medical emergencies of all wounds. These infections require prompt and even preventive attention with antibiotics when they emerge!
There are several bacteria responsible for creating serious infections in your system. They are Streptococcus (strep throat, scarlet fever) and Staphylococcus (staph) that can cause cellulitis and impetigo, methicillin-resistant Staph aureus, Hemophilus influenzae, Pneumococcus, and Clostridium species. Lymphangitis, which is an infection of the lymph vessels can develop, can also be caused by the Streptococcus bacteria. If left untreated, it can spread to the skin, causing cellulitis, or into the bloodstream, causing septicemia, or sepsis.
Sepsis
Sepsis is a very serious condition that develops quickly and requires immediate medical attention! Sepsis and septic shock can occur from any bacteria infection, very commonly from cellulitis, pneumonia, influenza and urinary tract infections (UTI). Even after treatment sepsis may contribute to chronic fatigue and pain, organ dysfunction or possible amputations. (1)
Lymphedema Bacterial Infections – Cellulitis
The difference among such infections occurring among the population with lymphedma, as opposed to those without lymphdema, is dramatic. (2)
- In Stage 1 lymphedema the incidence of infection is 1 per 100 patients, or 1,000 times greater than the normal population.
- In Stage 2 lymphedema the incidence is 27 per 100 patients, or 27 greater than Stage 1.
- In Stage 3 lymphedema the incidence is 72 per 100 patients, or about 3 times greater than Stage 2.
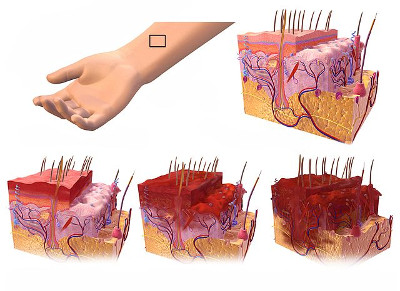
The most common bacteria infection that affects those with Lymphedema is cellulitis. Cellulitis affects all layers of the skin and can present fairly quickly. Symptoms of cellulitis, which mainly occurs in the legs of those with lymphedema are:
- Redness and warmth of the affected tissues (look and feels like a bad sunburn)
- Streaky red lines on the skin
- Increasing swelling and pain in the affected area (think sunburn feeling)
- Chills and fever (as your body tries to fight this serious infection)
- Malaise and having flu-like symptoms (including vomiting or diarrhea)
- Swollen lymph nodes (sign your body is fighting to contain the infection)

If you see or experience any of these symptoms, especially the tell-tale sunburn like symptoms you need to see a medical professional as soon as possible for antibiotics! Ideally, the protocol of those suffering with Lymphedema is to have a bottle of antibiotics on hand at home so they can be taken immediately without delay! Most people will respond well to oral antibiotics while others may need stronger antibiotics usually administered via and IV line. Timing is very important when getting treatment.
Cellulitis Treatment
The following are some examples of antibiotics that have been used to treat cellulitis and co-occurring bacterial pneumonia caused by the same strain of bacteria (3)(4):
- Penicillins (Intravenous or oral)
- Amoxicillin
- Amoxicillin and clavulanate (Augmentin)
- Ampicillin and sulbactam (Unasyn)
- Piperacillin and tazobactam (Zosyn)
- Cefazolin (Intravenous)
- Cephalexin (Keflex)
- Ceftriaxone (Rocephin) (Intravenous)
- Cefuroxime (Ceftin, Zinacef)
- Ceftazidime (Fortaz, Tazicef)
- Clindymacin (Intravenous)
- Azithromycin (Zithromax, Zmax)
- Erythromycin (Erythrocin, E.E.S., Ery-Tab, EryPed)
- Imipenem and cilastatin (Primaxin)
- Levofloxacin* (Levaquin)
- Ciprofloxacin* (Cipro)
- Vancomycin
Important Note on Fluoroquinolones
The drugs asterisked above belong to a group called fluoroquinolones, which are a broad spectrum antibiotic mainly used to treat respiratory and urinary tract infections. The fluoroquinolones used in the United States include ciprofloxacin, gemifloxacin, levofloxacin, moxifloxacin, norfloxacin, and ofloxacin. These antibiotics come with a “Black Box” warning from the FDA (Food and Drug Administration) on the dangers in taking all forms of this class of drug. It can cause very serious side effects, which can be permanent and include tendinitis and tendon rupture (particularly in the Achilles tendon), liver problem such as hepatitis, mood and mental changes, pain, swelling, tremors and more. (5)
It is strongly advised those with EDS (Ehlers Danlos Syndrome), particularly those with hypermobility (regardless of a hEDS diagnosis), avoid taking any of the antibiotics in this group. These drugs should be reserved for the severest conditions where life is being threatened. It can cause a cluster of conditions known as “floxing” in the EDS community. Due to weak connective tissues, as is also found in those with Lipedema (so it would be double dipping for us), these drugs would further degrade our tissue connectivity causing tendon ruptures, gastric problems, mental changes and lots more. Some of these changes could last for weeks, months, years or even be permanent! I strongly urge you to discuss this topic with your medical team to avoid bein “floxed”!
Getting Treatment
In all cases, physicians choose a treatment based upon many factors, including the location and extent of the infection, the type of bacteria causing the infection, co-occurring conditions, your medication allergies, and your overall health status. Of course, be sure to tell or remind the treating medical professional of any allergies you have to proposed antibiotics! You don’t want to make a bad situation worse.
If you cannot start treatment right away further complications will develop, such open wounds, ulcers or necrotizing fasciitis, which will require advanced treatment from your wound care clinic. This will involve more pain, temporary limited loss of limb functionality, additional topical medications, bandaging and maintaining a constant vigil to ensure the wound is healing and not succumbing to further infection.
Personal Note 1: I had a strep throat in 2008 that was treated with Cephalexin, which turned out I was allergic too and ended up in the hospital fighting a medicinal allergy and untreated strep. The strep toxin settled in my legs creating a bout of cellulitis. It all happened so fast that I had a pic line installed in my left arm and chose to treat at home, giving myself multiple antibiotic injections each day for several weeks. A large deep ulcer developed on the back of my lower right leg that almost had to be cut out because we couldn’t find a treatment to stop the bacteria growth. Our last attempt worked and it took over six months to heal the ulcer. I’m sure many of you know what I am talking about!
Personal Note 2: I had a cellulitis infection twice in 2022 that went septic and I had to be hospitalized. The same bacteria infection that caused the cellulitis also caused bacterial pneumonia. They gave me IV antibiotics for 6 days and oral antibiotics for two weeks after that to clear both infections. It was a total of four different antibiotics to treat both conditions, which destroyed my gut! I had blood draws at least twice a day to monitor my sepsis infection. I have noticed that a day before a bright red rash appears I become violently ill, vomiting and diarrhea, with extreme fatigue, slight temperature and body aches (much like the flu). That is my queue to get to the hospital quickly to start treatment!
Personal Note 3: I had pneumonia spring of 2022 and the emergency room doctor prescribed Levofloxacin (generic form of Levoquin). I refused but was told it was the only drug they were prescribing for pneumonia, especially as I am allergic to several antibiotics. Being too sick to argue I reluctantly accepted it, went home and took my five day course. On day four I started experiencing many of the “floxing” symptoms, including pain and weakness in both my Achilles heel tendons preventing me from walking. I also had confusion, extreme fatigue, formication, nausea, diarrhea and other symptoms. I was bedridden for weeks fighting my way back to health. I still have weak ankles, fatigue and brain fog that I continue to battle. “Floxing” is very real and can be quite debilitating for the short and long runs!
Healing Your Gut
If you need to take an antibiotic regimen, which may include intravenous and or oral treatment, for any length of time it may destroy much of the good flora in your stomach. This may lead to bloating, stomach pain, nausea, vomiting, diarhhea (which can be uncontrollable), inability to hold much food in your stomach and tolerance for only bland food.
This can lead to another very serious bacterial infection known as C. Diff (Clostridioides difficile or C. difficile). If you continue to have diarhhea for several days along with colitis condition, your doctor may order a stool test to test for the presence of this bacteria. Ironically if you test positive for C. Diff your doctor will prescribe another antibiotic to kill the infection.
Antibiotics are necessary for treating many bacterial infections in the body, especially if you have a life threatening condition. The downside to antibiotics is the destruction of the good flora in your gut biome which shifts the balance in favor of the bad bacteria in your gut and digestive track. This can cause frequent stomach pain, difficulty eating and digesting any food, diarrhea, bloating, skin issues, start of autoimmune conditions, weight gain, food cravings and trouble sleeping.
There are steps you should take to start healing your gut quickly as it can take up to six months to rebalance your gut biome. Taking a Probiotic with strains of the Lactobacillus family can help rebuild the gut biome. (6) (I took a Culturelle Probiotic two to three hours after taking an antibiotic and normally take one daily to help keep my biome balanced.) You can also eat natural foods with prebiotic or probiotic properties that help foster the growth of good gut flora, such as kefir, fermented items like sauerkraut and kimchi, greek yogurt, pickles and Kombucha, eating fiber-rich whole foods, garlic and bananas. Rebalancing your gut and intestinal microbiome is critical to the proper function of all systems in your body, including maintaining the best level of immunity!
Takeaways on Skin and Wound Care
People with Lymphedema, especially those with advanced stages, are at high risk of wounds occurring in compromised skin areas. You need to be prepared to treat these injuries or infections or have an emergency plan for treatment at your doctor’s office or emergency room. Tell your treating medical professional that you have Lipedema and Lipo-Lymphedema. Be prepared to explain your condition(s) as doctors are not well versed in fat and lymphatic systems.
 Assemble and keep a first aid kit at home suitable to treat your condition. In addition to the standard kit you may want to include non-allergic medical tape, assorted gauze size bandages, neosporin (or other topical cortisone or antibiotic cream), and your emergency antibiotic prescription for bacterial infections.
Assemble and keep a first aid kit at home suitable to treat your condition. In addition to the standard kit you may want to include non-allergic medical tape, assorted gauze size bandages, neosporin (or other topical cortisone or antibiotic cream), and your emergency antibiotic prescription for bacterial infections.
Personal hygiene is essential to preventing fungal infections, skin tears and wounds in fold creases and reducing areas where bacteria might enter your body. Cut your toe and finger nails short to avoid accidental scrapes, cuts and itching of your skin. Keep your skin hydrated and use special moisturizers to repair dry skin and lock in hydration, such as Eucerin or CeraVe.
Take good care of your beautiful self and body. You know best what looks and feels normal. Always check in with your medical professional(s) whenever something looks or feels wrong with your body. A cellulitis or sepsis infection requires timely treatment to avoid critical complications, including death!
To your improved health!
References:
- (1) Sepsis Alliance – Cellulitis
- (2) LymphNotes.com – Lymphedema Related Infections
- (3) MedicineNet.com – Cellulitis
- (4) Centers for Disease Control – Group A Streptococcal (GAS) Disease – Cellulitis
- (5) National Library of Medicine: National Center for Biotechnology Information – FDA Adds “Black Box” Warning Label to Fluoroquinolone Antibiotics
- (6) National Library of Medicine: National Center for Biotechnology Information – Effects of probiotics on gut microbiota: mechanisms of intestinal immunomodulation and neuromodulation
I have lymphedema in both legs. I recently fell and scraped one leg on carpet. It drained, which burns horribly. Have been to the ER, am taking antibiotics. But no one can seem to answer my questions: will this Heal and stop draining? If so, how long should it take? 2 weeks, 2 months? 6 months?
Hi Ruth!
I am so sorry you fell and hurt your leg badly! Having wounds in legs with lymphedema can be very trying. You need to be very vigilant for signs of infection and to keep the area very clean. I cannot see the wound, but a course of antibiotics sounds like a good precautionary measure to minimize risk of infection and cellulitis. Are you elevating your wounded leg as much as possible? Are you bandaging it or leaving it open? I had to be seen at the Wound Clinic for special topical medicine to sterilize and heal the wound. It took three different ointments before I found the one that worked on my wound. I can’t say how long it will actually take to heal, but mine took six months. Your body may take longer than normal given the severity of lymphedema in the legs.
The ER is a great place to get immediate urgent medical care for your wound. However, I would suggest you follow-up with your Wound Clinic and have them evaluate it for long-term monitoring and treatment. They are the best group equipped to handle your wound needs.
Wishing you a speedy and complete healing!!
Esther