CDT: Compression Bandaging and Technologies
Compression bandaging, garments and technologies are a necessary part of the Complete Decongestive Therapy (CDT) treatment for Lipedema and Lymphedema. Applying and maintaining the correct compression solution has many proven benefits. These include alleviation of pain from swelling, maintenance and reduction of pooled lymph fluid, and reduction, elimination or prevention of fibrotic tissue buildup. There are several things to consider before choosing a compression solution for your needs. Let’s look closer at CDT: Compression Bandaging and Technologies solutions.

Warning: If you suffer from venous insufficiency, cardiac issues, open wounds or other health conditions, moving large volumes of fluid around the body, especially into your trunk area, might have negative consequences. Please consult your physician, your Certified Lymphedema Therapist (CLT), or physical therapist prior to using compression bandaging.
The Need For Compression Bandaging or Garments
Compression is a mechanical process that provides equal or greater pressure evenly via a bandage, garment or pump to prevent further swelling of an affected body part, usually one or more of the limbs. Unlike normal compression, graduated compression applies the greatest pressure at the point furthest from the heart, the distal point, and decreases as you move towards the end of the bandage or garment, the proximal point.
Depending on the pathology, medical compression therapy can be applied in different forms: socks, stockings, tights, bandages, specialty garments or pumps. A skilled Certified Lymphedema Therapist (CLT) or physical therapist will evaluate your situation and prescribe a compression technology that is best suited for your unique needs. The type of compression garment(s) needed will depend on multiple factors including, size and shape of affected area(s), the presence of lymphedema, the presence of one or more shelves or lobules, the condition of the skin, allergies, ability to don garments yourself, the type of compression required and other extenuating medical conditions. We will explore these in greater depth in this article.
Compression Concept
The use of compression bandaging, garments or pumps for Lipedema purposes is to minimize the area of growth, usually in the legs, and provide temporary pain reduction resulting from swelling of the tissue areas around the Lipedema fat. For those in the early stages of Lipedema, you might only need an uniform compression garment with minimal pressure gradient to effectively manage your affected area(s).
If you are in the more advanced stages of Lipedema, you might need to use a graduated compression garment. By compressing the limb(s) with graduated compression — strongest at the ankle and decreasing up the leg — the compression stocking or garment helps with:
- venous return,
- decreasing venous pressure,
- preventing venous stasis,
- reducing edema and deterioration of venous walls, and
- efficiently relieving aching and heavy legs by aiding the body in moving blood up the leg.
This treatment is prescribed by a clinician to treat lymphedema, phlebitis, thrombosis, aftercare following surgery, sclerotherapy, and any other forms of varicose vein treatment. It is also prescribed to relieve all conditions of chronic venous disease (heavy legs, varicose veins, edema, and leg ulcers). It can also be prescribed to prevent venous issues during pregnancy and long distance travel. If no contraindications exist, like severe arterial insufficiency are present, you may even buy compression stockings of lower pressure without prescription.
The Need to Treat Co-Occurring Lymphedema

Lipedema usually involves both limbs.
Lymphedema causes additional inflammation, swelling and pain the affected limb(s), which can exacerbate the Lipedema condition. The excess lymph fluid trapped in the limb(s) is a combination of the body’s waste materials from proteins and fats (chyle), water, and white blood cells (lymphocytes), which is intended to travel up to the chest and abdomen area for processing out of the body. When it becomes trapped and stagnant, it turns into a breeding ground for bacteria (risk of cellulitis) and fibrosis (thickening and hardening of the tissues). (1)
The presence of lymphedema makes wearing compression garments even more imperative. Left untreated the affected limb(s) will continue to grow in size and shape creating large pockets of fluid, known as lobules and shelves, which will increase the risks of infections, tissue damage, limb deformity, gait changes and possible immobility. In addition to compression garments, manual lymph drainage (MLD) therapy, and dietary changes you may also need to use a pneumatic compression device or pump.
Compression Gradients
Compression garments are normally prescribed or purchased based on the recommended pressure gradient. The gradient is determined by the amount of pressure exerted on the skin by the sub-material of the garment and can be affected by the elasticity and material of the garment. Gradient pressure can also be affected by the size and shape of the person’s legs as well the type of movement of the limb.
They are categorized into classes measured in millimeters of mercury (mmHg) as follows:
- 15-20 mmHg
- 17-21 mmHg
- Class I: 20-30 mmHg
- Class II: 30-40 mmHg
- Class III: 40-50 mmHg
- Class IV: 50-60 mmHg

Graduated compression garments should be discussed and selected with your physical therapist, doctor or specialist. Randomly choosing a garment can result in either an ineffective compression solution from being too loose or create additional pain and damage to the affected area by being too tight!
Contraindications For Compression Garments
Compression garments are a necessary tool for those with Lipedema or lymphatic disorders. However, there are circumstances when compression garments should not be used without approval from your medical professional or physical therapist. Some of those contraindications include (2):
- Suspected or proven peripheral arterial disease, including history of peripheral arterial bypass grafting
- Severe peripheral neuropathy or other cause of sensory impairment
- Allergy to stocking material
- Massive leg edema or pulmonary edema from congestive cardiac failure
- Local skin or soft-tissue condition, including recent skin graft, fragile “tissue paper” skin, gangrene, oozing dermatitis and severe cellulitis
- Extreme deformity of the leg, or unusual leg shape or size preventing correct fit
Types of Compression Garments
There are many forms of compression therapy, which include elastic and non-elastic bandages, boots, hosiery or stockings, and pneumatic devices. Graduated compression stockings are commonly prescribed, are generally more acceptable, and relatively easier to don and doff than traditional bandaging and pneumatic devices. However, those prescribed graduated compression stockings may not tolerate them well and require a different solution. The effectiveness of a prescribed solution is only defined by the compliance of daily use, so it is important to find the right solution for those who need a compression garment. (2)
Selecting an appropriate compression garment is probably the most challenging task in Lipedema and Lymphedema treatment. It is important to begin the discussion of garments early in the course of treatment. It often takes time for patients to adjust to the fact that they will need a garment. Physical Therapists must also ensure their patients will adhere to their wear in order to determine the effectiveness of the prescribed solution.
In many instances, patients must pay all or part of the cost of the garment, and they will need to plan in advance for the expenditure. Planning should also extend to replacement compression garments as most need to be changed out on a regular basis, so their future cost must be factored into the financial outlook. Important factors to consider when choosing a compression garment are:
- coverage, compression class,
- appearance,
- custom-made versus ready-made (off the shelf),
- material,
- construction,
- suspension,
- skin condition/sensitivity,
- donning/doffing, and
- cost and source of payment.
These garments are usually available “off the shelf” and are measured in the ankle, calf and thigh areas. The higher gradient should be in the ankle, or distal point, and tapers off as you move up the garment. It is imperative you measure your limb accurately and ensure the tightest compression is at the ankle so fluid moves up the leg from the ankle to the knee to the thigh and up into the trunk for processing. If your tightest point is at the thigh then fluid will flow backwards into the lower leg where it will pool and not drain out of the leg.
Let’s look at the different types of compression bandaging and technologies currently be used to treat Lipedema and Lymphedema.
Short Stretch Bandages
Your Physical Therapist may start compression on your limbs using short stretch bandaging to reduce as much edema in your limbs as possible before determining the best long-term garments for your needs. These bandages, which are usually applied in layers, provide both compression and high resistance to stretch to increase venous and lymphatic return.
Patients usually wear a stockinette under the bandaging to protect the skin from irritation. Textured or stiff smooth foam is used under the bandages to increase the resistance and provide a gentle massage to assist in breaking up fibrosis and to stimulate lymphatic drainage. Foam and cotton batting may also be used to fill the areas under a shelf, lobule or sensitive areas to give your limb a conical shape, which facilitates effective bandaging.
Properly layering of compression material will yield the best results in reducing and maintaining your leg size. They should be applied in the following and may vary slightly depending on the severity and shape of the lymphedema. Items in parenthesis are the items I use.
- Lotion – to keep your leg(s) moisturized and reduce skin breakdown (Eucerin Intensive Repair)
- Stockinette – to protect your skin from foams and garment and from lotion getting on to your expensive garments. If you use velcro close garments you may want to put another stockinette over to prevent the velcro of both legs from sticking to each other. (Stockinette)
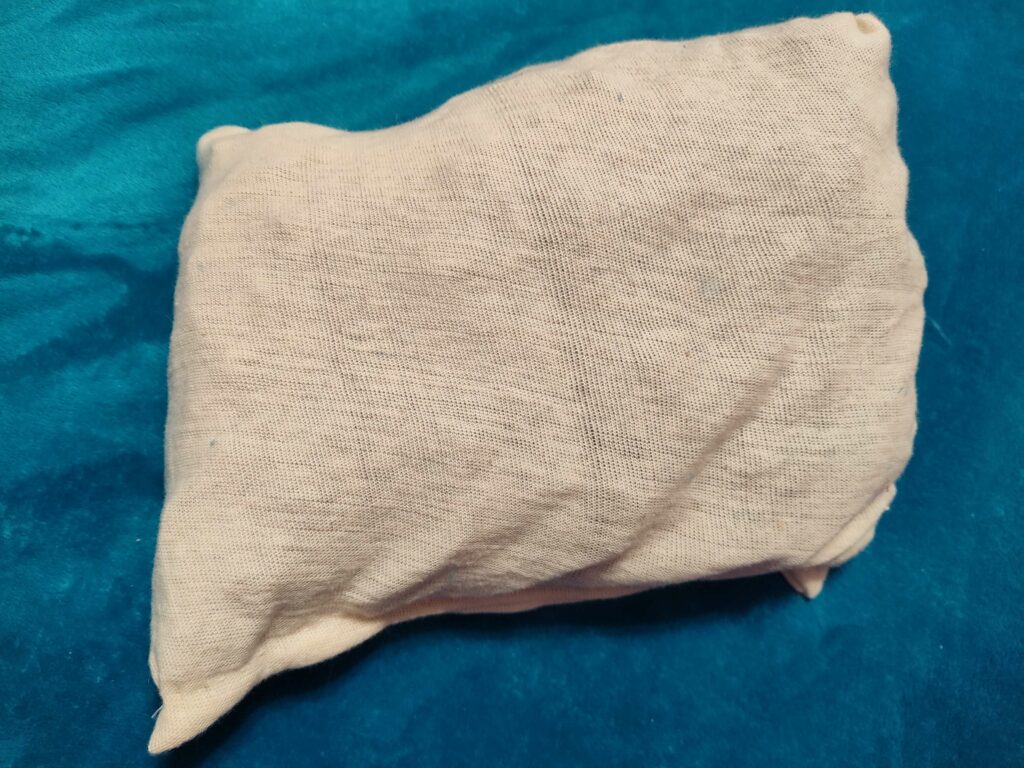
- Chip bag – some may have stubborn edema or fibrosis in specific areas of the leg(s) where applying a chip bag is beneficial to gently massage area (I make my own homemade chip bags.)
- Foam(s) – some may need a light foam to pad and fill in crevices while others need thicker foams to provide greater resistance with the lighter foam wrapped over top to hold the thicker foam in place (cut gray sheet foam and thin foam to hold in place, homemade chip bags under the foam)
- Short-stretch bandages – specialized bandages, which come in several sizes and lengths, to hold all underlying layers in place and maintain lymphedema in the leg(s). Comprilan and Rosidal are the two most popular brands. (Both work gYoureat. I use the 6cm x 10m for the foot, the 8cm x 10m for the ankle and 12cm x 10cm for the legs. I do NOT use the clips provided as they don’t hold well and will poke the skin if nothing but stockinette is below. I use masking tape and rip my pieces ahead of time for easy taping at the end of each bandage.)
You can see more options on the Product Resource Page under the bandaging section.
Brands: Comprilian and Rosdial, Foams and Padding, Stockinettes
Circular Knit
Circular knit garments are made of nylon and are thin in nature. They have no seam to dig into the skin as they are made in a circular fashion. These type of garments are not suitable for those with larger or non-conical shaped limbs. The garment will tend to bunch up in the creases creating a tourniquet effect. This can cause extreme pain and result in skin infections, skin tears or possible blood clots from increased artificial pressure.
Brands: Medi USA, Sigvaris, Jobst, Solidea, Solaris, Juzo, Other
Flat Knit Garments
Flat knit garments are normally thicker in size over circular knit garments. They are made flat and sewn together in the back of the garment with a seam. They can be different densities as some are made with nylon while others are made with cotton blends and others have a heavier wool type feel. Flat knit garments tend not to bunch in small creases, so can be used on non-conical legs.
These garments are custom made and thus generally more expensive than circular knit garments. You will need a therapist or specialist to custom measure your limb(s) to ensure the garment(s) meets your needs. Check with your medical insurance to see if they will cover the costs of these garments. Sometimes the patient may need to pick up 100% or a partial cost for the garments.
Tip: always measure at your smallest size to ensure the best fit. For many people it is first thing in the morning before swelling begins.
The material can be made into lower leg garments, thigh highs, pantyhose style, capri cuts or other shape needed to fit your unique limbs. The gradient of these garments is similar to regular compression bandages.
Brands: Juzo, CzSalus, Jobst, Medi USA, Solidea, Sigvaris
Inelastic Velcro Systems Garments
These garments are made of thicker little to no stretch fabric. They offer more support and are great for post-operative care. The garments often involve the use of neoprene or velcro to secure the garments. While neoprene can be slightly resized, accurate measurements are necessary to ensure proper fit for the shape of your limb.
These garments are a great option for larger limbs that require more secure support. They employ velcro straps that can be readjusted throughout the day to keep the garment tight thus ensuring proper compression. Those that suffer with Lipo-Lymphedema can find these garments for both lower leg and upper leg solutions.
Brands: CircAid, Juzo, Solaris, Jobst/Farrow Wraps, Sigvaris
Inelastic Velcro Systems Garments – Specialty
There are specialty custom compression garments available for those who are stage 4 Lymphedema or stage 4 Lipo-Lymphedema that have abnormal pockets of fluid called lobules or lobes. These lobules usually preclude people from choosing standard off-the-shelf garments and require a lymphedema specialist to properly measure your leg(s) to order a custom made garment(s). Be prepared to pay more for custom made garments, which can run $300 in a co-pay situation up to $5,000 (or more) per pair without insurance coverage. Work with your medical team to identify possible financing options or ways to reduce your co-payment amount.
Brands: Medi USA / CircAid, Sigvaris
Micro Massaging Garments
These garments are specially designed in a “knit wave” pattern that massage your limb as you move. You should see a slight imprint of the garment pattern on your limb as certification the compression and massage is working properly. However, you need to be sure the garment is not too tight and “cuts into” your skin, creases or shelf areas.
Garments are available knee high, thigh high, pantyhose, capri and shorts sizes. Sizing on these garments is limited. This means larger sized patients may not be able to purchase these garments to fit their affected limb(s). They may also not be a good choice if you have very large shelves or lobules.
Brands: Solidea (up to 2XL), Bioflect (up to 5XL)
Night Time Compression
Compression garments used during the day are usually not appropriate or recommended for night time use. They are too tight, prone to slippage and may bind in creases causing a tourniquet effect while you sleep. Consult your physical therapist to see if you need to wear night time compression garments and which type will work best for your needs. Reasons for wearing a night time compression garment(s):
- reduced daytime edema returns after a night’s sleep
- there a patches of fibrotic tissue that could use a gentle massage at night
- you wear customized compression garments during the day
- edema reduction at night makes donning daytime compression garments easier.
CircAid, Sigvaris and JoviPak make foam compression sleeves to be used at night.
Garment Care
It is important to properly care for your compression garments to ensure longevity and proper operation. Most people approved for compression garments may only be allowed to replace them once or twice a year, which makes maintaining their integrity vital for your daily needs. Some people may purchase a second or third set of garments to rotate through the wash and extend the compression abilities of each garment. This may work for off-the-shelf garments and short stretch bandages. Custom made garments may be too expensive to afford an alternate set, so maintaining them is paramount to continued edema reduction efforts!
Stockinette(s) and short stretch bandaging can be washed by machine and air dried to maintain shape. Tights, pantyhose, capri and legging garments can be easily laundered too. Custom garments and non-elastic garments will come with cleaning instructions. Keep the garments clean of dirt and bacteria from sweat and wound leakage. Be sure to keep your velcro tabs clear of debris to ensure they close and hold your straps securely.
Budget money for replacements. Garments usually last four to six months if used on a daily basis. Consider using two sets of garments, especially short-stretch and non-custom garments, alternating between the sets. This will allow you to launder one set while wearing the other set.
Complications of Graduated Compression Garments
It is vital your compression or graduated compression garments fit your affected area(s) correctly. Garments that are too loose or too tight, improperly sized, improperly donned or use fabrics that affect your skin can cause complications, some even life threatening.
Here are some commonly seen problems when using compression garments:
| Condition | Action |
| Garments are too tight (Could cause DVT, neuropathy or nerve damage, ulcers, skin necrosis) | Check they are donned correctly; loosen straps, remove any unnecessary bulky undergarments; discuss sizing problems with therapist. |
| Garments are too loose (area continues to swell) | Check they are donned correctly; pull straps tighter; insert foam fillers into loose fitting areas; discuss sizing problems with therapist |
| Itchy skin or rash | Possible allergic reaction to one or more garment materials; try using cotton stockinette under garments to protect skin |
| Skin is bulging | Check they are donned correctly; are straps tighter at top of garment than bottom causing edema; signs of venous insufficiency |
| Oversized shelf, lobule or fat pad (garment may bunch up in crease below shelf creating a strangling effect!) | Several garment manufacturers custom make garments to fit over/around irregularly shaped limbs to aid in their compression; redo your bandaging if it bunches up in the area below your shelf to avoid cutting off circulation or creating a DVT. |
| Area is hot to touch or turning red | Seek medical attention as this could be signs of cellulitis or other infection |
It is imperative that your compression garments fit well, even if you have irregularly shaped limbs, and can be donned easily. It is also important that you wear them as prescribed. The compression garments can only benefit you if you wear them on a regular basis!
Communicate regularly with your therapist about your progress and if you experience any problems, especially as outlined above, with your garments. They have techniques, such as using custom foams, chip bags, stockinette materials and emollients to help with proper form fitting and skin protection. (I learned quite a bit from my physical therapist!)
Additional Compression Technologies
Compression garments are a great way to reduce or maintain a limb(s) affected by excessive Lipedema fat. However, if your lymphatic system has become impaired you may require additional assistance moving the excess fluid out of your limb(s). This excess build-up of lymph fluid in the limb(s) is known as lymphedema and is quite common in the advanced stages of Lipedema and those sustaining deep wound damage to a limb or trunk area.
Lymphedema Pump
A doctor or physical therapist will generally prescribe a pneumatic compression device, known as a lymphatic pump, to include in your care routine to treat lymphedema. This could be a temporary situation, such as post-surgical support, venous support during pregnancy, or as prevention for long distance or air travel. However, compression devices are generally recommended for those suffering with chronic conditions, such as lymphedema, lipo-lymphedema, and venous diseases (varicose veins, heavy legs, and leg ulcers).
Lymphedema pumps and the associated sleeve(s) can be purchased off the shelf but may be covered under your medical insurance plan. You will want to investigate your coverage options as pumps can run from a couple hundred to a couple thousand dollars depending on the type you need. The sleeve(s) you use with the pump may need to be custom made too, which can be expensive.
A trained physical therapist should choose the correct size and type of pump and corresponding sleeve(s) that fit your unique needs. Some pumps provide uniform air pressure in each sleeve segment that can have between three and eight chambers. Other pumps use an automated air gradient pressure system that applies a higher pressure at the distal point (furthest from the torso) decreasing in pressure until it reaches the proximal point (closest to the torso).
Sequential pumps apply pressure at the distal point and “hold” that pressure as each sequential chamber inflates. The pump deflates the sleeve(s) when the distal pressure has been applied. Peristaltic pumps apply pressure at the distal point and sequential move up the sleeve to the proximal but does not “hold” the pressure in the previous chamber. This is ideal for sensitive patients or those with wounds. The combination of pump type, pressure choice and number of segmented sleeve chambers needs to be carefully evaluated to provide you the best and safest fluid reduction strategy possible.
Be sure the pump you buy or rent is for lymphedema purposes and NOT a massaging unit! These devices may look similar, but will NOT provide amount or type of pressure needed to properly address your Lymphedema.
Examples of compression pumps include:
 | Bio Compression Pumps Pumps are four or eight segments that provide distal to proximal sequential lymphatic movement. Supports one or two sleeve options. Learn more – Bio Compression Pumps |
 | Medical Solutions Provider Lympha-Press pumps encompass both sequential and peristaltic therapies to accommodate sensitive people and those with wounds. Pumps support arm and legs sleeves as well as their patented “pod” device to accommodate larger patients and those needing to include abdomen and genital areas. Learn more – Medical Solutions Provider |
 | Tactile Medical FlexiTouch pumps provide sequential compression from the distal point to the proximal point. Garments are available in half leg, full leg and full leg with abdominal support and options for the upper body. Learn more – Tactile Medical |
Kinesiology Tape
Kinesiology tape is about the same thickness and elasticity that mimics human skin. As the limb moves the tape adhesive gently lifts the skin underneath stimulating blood flow and lymph fluid movement. Studies have found kinesiology tape can be an effective tool for those with early-stage lymphedema, especially if other compression technologies are not tolerated well. (3)
The success of lymphedema movement and reduction with kinesiology tape largely depends on how it is strategically placed on the body. Patients should work closely with their physical therapist who is trained in the use of kinesiology tape for lymphedema. Normally the tape is applied in a fan pattern over lymphedema areas and is most effective when combined with patient movement, such as cycling, walking or swimming, to maximize lymph fluid movement.
Note: kinesiology tape has not been adequately studied for patients with Lipedema and lymphedema, but has shown promising results for reducing early edema due to surgery or injury trauma. Kinesiology tape may not be an option for people who have tape or adhesive allergies. Always consult with your Physical Therapist before trying a new technology to avoid damage to your system.
Tips and Tricks
Some people may find the compression maintenance regimen arduous and frustrating at times. There may be steps that are difficult to perform or areas of treatment that don’t seem to make any progress. This may lead to people foregoing the necessary steps of treatment and abandoning the whole maintenance process. Here are some tips that might help tackle some of those challenging steps.
Chip Bags: if you have one or more fibrotic areas where pumping and wrapping are not helping, try using chip bags. Chip bags contain two to three different density foams chips usually cut into 1″ x 1″ squares and stuffed into a soft bag that can be used inside compression garments or inside a sleeve used with a pneumatic pump. The movement of the leg or graduated pressure of a pump gently massages the fibrotic area, simulating human massage only longer.
Chip bags can be purchased premade (with chips or channeled foam) or you can purchase pre-cut chip pieces to make your own chip bags. You can also make your own chip bags in the shape or size needed by cutting a piece of stockinette material, sewing the end, inserting cut up foam, and sewing up the open side. You can use foam from seat cushions mixed with stiffer foam density of gray sheet foam or orange foam from a craft store or lymphedema store or wavefoam. Make sure the foam is clean and free of stains, mold or bacteria before considering it for your chip bag.
—–> Learn How to Make Your Own Chip Bag <—–

Donning and Doffing Garments: putting compression garments on and taking them off can be a very challenging task! This is probably the top complaint therapists get when outlining a treatment regimen for lymphedema patients. There are professional tools you can purchase to assist in the donning and doffing process. I prefer to use my trusty grabber tool to pull my compression sleeve over my foot and lower leg. It works well for this task in addition to other things I need to reach or grab. It is one of the cheapest and most used tools in my toolbox!
If you are donning and doffing circular or flat knit garments you may want to use a pair of gripper gloves. This will allow you to keep a firm grip on the garment and avoid puncturing it with your finger or nail. You may also want to roll each leg down to the foot to essentially roll the garment up your leg as you don it.
Please let me know if you have any tips or tricks you can pass on to others to make it easier to maintain their complete decongestion treatment regimen!
CDT: Compression Bandaging and Technologies Summary
Compression bandaging, garments and technologies are a necessary part of the Complete Decongestive Therapy (CDT) treatment for Lipedema and Lymphedema. These include alleviation of pain from swelling, maintenance and reduction of pooled lymph fluid, and reduction, elimination or prevention of fibrotic tissue buildup. Choosing the correct compression regimen is an unique process that should be discussed and approved by a Certified Lymphedema Therapist (CLT) or physical therapist knowledgeable in Lymphedema treatment.
The use of short-stretch bandaging along with various foam options is usually the first compression technique used to significantly reduce the Lymphedema in the leg(s). You may also require the assistance of a pneumatic pump to assist in fluid movement and the softening of fibrotic tissue. Once the Lymphedema is at a maintenance level, your physical therapist will recommend a compression garment that fits your needs. This could include a circular or flat knit garment for those with mild Lymphedema or Lipedema. However, you may require an inelastic velcro or custom garment if your Lymphedema is significant or severe.
Consistent monitoring and care of your garments is paramount to the ongoing success of edema management. Consult your physical therapist if you experience any problems donning or adjusting the garments. The daily wear of these garments should not cause pain, bunch up in a fold or be too tight. Garments should be laundered and carefully maintained to ensure the proper operation and longevity of your compression solution.
The CDT: Compression Bandaging and Technologies is one of a four-part complete decongestive therapy process. Please review the Skin Care, Manual Lymph Drainage (MLD) and Exercise sections so that you and your Certified Lymphedema Therapist (CLT) or Physical Therapist can formulate a complete CDT plan tailored to your needs!
To your improved health!
Resources
Videos:
- Fat Disorders Research Society – Compression Show and Tell #FDRS2016
- YouTube – Using Kinesiology Tape to Manage Lymphedema – How to Apply Kinesiotape to Reduce Swelling
- YouTube – Making and Applying a Chip Pad for Sub-acute or Chronic (Brawny) Edema
- YouTube – Foams and Padding for Lymphedema Bandaging: for edema and fibrosis treatment (Lymphedema Products)
- YouTube – Compression Bandaging For The Leg
- YouTube – Velcro Compression Wraps for Swelling and Lymphedema – Compression Garments Reviewed
- YouTube – Compression Stockings Reviewed & Explained by a Lymphedema Physical Therapist
Sites:
- Kinesio Taping – Kinesio Taping Of Superficial Lower Extremity Lymphatic Pathways
- National Library of Medicine: National Center for Biotechnology Information – Kinesiology Taping reduces lymphedema of the upper extremity in women after breast cancer treatment: a pilot study
Bandaging and Garment Shopping:
References:
- (1) US National Library of Medicine National Institutes of Health – Cellular and molecular mechanisms of fibrosis
- (2) US National Library of Medicine National Institutes of Health – Graduated compression stockings
- (3) US National Library of Medicine National Institutes of Health – Kinesiology Taping Reduces Lymphedema of the Upper Extremity in Women After Breast Cancer Treatment: A Pilot Study