What is Lymphedema?
Lymphedema or Lymphoedema (as it is known in the European community) is the collection of fluid, cellular matter and fat products from tissues that results in swelling of one or more limbs, neck, face or abdomen area due to a blockage in the lymphatic system. Unlike Lipedema that presents symmetrically on both sides of the body, Lymphedema usually affects just one limb or area. The most common form of Lymphedema is in the arm of women recovering from breast cancer. Let’s examine Lymphedema causes, stages, the lymphatic system and treatment further.
Lymphedema is also present in those suffering with Lipedema in Stage 4, which is why they call it Lipo-Lymphedema. Lymphedema can be slightly noticeable to disfiguring in those with the condition. While there is no cure for Lymphedema there are treatment options to reverse or minimize its expanse. The treatment involves using a defined Complete Decongestive Therapy (CDT), which includes skincare, manual lymph drainage (MLD), compression bandaging and technologies, and exercise to manage the swelling and movement of fluid out of the system.
Types of Lymphedema
Lymphedema is classified as either Primary or Secondary.
Primary Lymphedema
Primary Lymphedema is present at birth usually the result of a genetic defect that causes abnormal formation of the lymphatic vessels. While present at birth symptoms may not develop until later in life. Primary Lymphedema has been classified into three forms and depends on the age when symptoms appear. It is not known whether there is a genetic link to this condition at this time.
- Congenital Lymphedema – symptomatically affects mostly females at birth with a 20% prevalence rate. A small group of people in this group show a genetic connection, which is known as Milroy disease.
- Lymphedema Praecox – demonstrates between birth and 35 years of age and is the most common form of primary lymphedema. Symptoms usually occur in females during puberty.
- Meige disease or Lymphedema Tarda – symptoms appears after 35 years of age and is less common than the other two forms.
It is not evident at this time if Primary Lymphedema can develop in conjunction with Lipedema. (I cannot find any supporting material to link Primary Lymphedema with Lipedema.)
Secondary Lymphedema
Secondary Lymphedema is caused by an unavoidable obstruction of lymphatic vessels and nodes usually brought about by surgery or a traumatic event to the body, such as deep cut, burns, radiation, scarring, vein stripping, or removal of a body part. The most common Secondary Lymphedema in the United States is from breast cancer. The combination of invasive surgery, coupled with chemotherapy, radiation therapy and removal of surrounding lymph nodes, damage surrounding lymph vessels and nodes causing swelling in the corresponding arm.
Those with Lipedema usually suffer with Secondary Lymphedema when fat clusters grow large enough to block existing lymph nodes and vessels.
Understanding the Lymphatic System (Basics)
The lymphatic system is one of least studied but most important parts of the human body. It is a major part of your cardiovascular system and responsible for half of what keeps your body in homeostasis, or in balance. It is responsible for recycling used fluid (much like a garbage collection system), inspecting all objects flowing through its borders for invaders, like germs or cancer cells, and calls out the cavalry, your immune system, when invaders are detected.
Whether you are suffering from Lymphedema or Lipedema induced Lymphedema you need to have a cursory understanding of what is happening in your lymph system. Your body is a remarkable machine. It has always fascinated me how all these systems work together behind the scenes to keep you healthy, moving, digesting, breathing, healing and feeling everything around you. Let’s see if I can do a high level overview so that you can appreciate what is (and in some cases isn’t) happening inside your body. You can also watch this great Patreon video for a quick overview of the Lymphatic System too.
In school you probably remember lots of talks and movies about your heart and how it pumps blood throughout your body, carrying food, oxygen and water through arteries and capillaries and then returns it to your heart to repeat the process. What you probably didn’t cover was what happens when food and fluid is dropped off to the cellular areas and how the waste is processed. This is where the lymph system comes in.
Blood carrying oxygen, food (proteins) and water travels from the heart to large arterial vessels all the way down to smaller vessels, capillaries, by way of a powerful high pressure system. This high pressure keeps the contents of the vessel from leaking out until it reaches an area of lower pressure, which is down in the thousands of capillaries in your legs, feet, arms, hands and other body parts. Your capillaries, which are semi-porous in nature then leak out oxygen, plasma, small proteins and water providing nourishment to surrounding tissue cells. The fluid builds up is the area between the cells, called extracellular fluid, until the pressure becomes too great and the fluid is forced into a surrounding lymph capillaries.
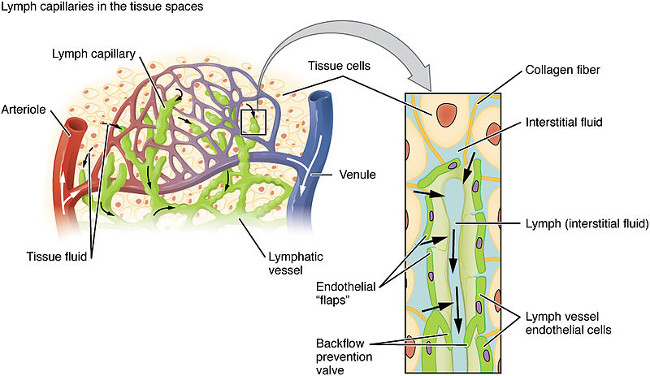
Lymph capillaries are intertwined with blood delivering and returning capillaries ready to pick up the waste products and return them into the bloodstream via larger lymph vessels. Lymph capillaries are unique in that interstitial fluid enters the capillary by a change in osmotic pressure via a one-way valve (cannot leak back out into the interstitial, or the between cellular space) where it begins its journey back to the bloodstream. Once the collected fluid and cellular matter is in the lymph capillary it is now called lymph fluid.
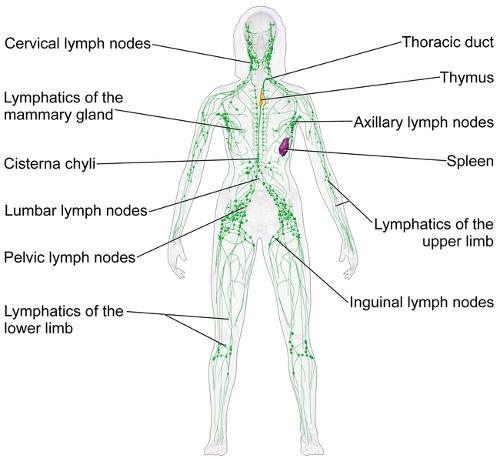
Lymph capillaries dump their contents into surrounding larger lymph vessels, which then are filtered through a lymph node. Lymph nodes are checkpoints where the fluid is inspected for infectious material. If found the offending material is quarantined in the node and reinforcements are called to try and eradicate the material. This is why you sometimes feel a large bump in your neck or under your arm. It’s your lymph nodes trapping identified bad material that cannot be allowed to re-enter your bloodstream.
Clean lymph fluid continues its journey through other lymph vessels, by means of muscle and body motion to propel it, until it reaches one of the two major lymphatic ducts – the right lymphatic duct and the thoracic duct (the left lymphatic duct). These ducts then drain into the right subclavian vein and left subclavian vein respectively, which are two separate and unequal drainage areas. The right subclavian vein receives its cleaned lymph fluid from the right side of the head and right arm area while the left subclavian vein receives its cleaned lymph fluid from the left side of the head and remaining body area. Now the process begins again.
As you can see from the above explanation the circulatory system is a closed system meaning the process of producing nutrient rich blood ends in the recycling of the spent blood at the same point with the process repeating numerous times per day. The heart beats powerfully strong and hard to move blood to the extremities of your system and back. The lymphatic system on the other hand is not a closed system nor does it have an equivocal heart to pump its fluid to the two drainage areas. Thus it relies on muscle, body and internal pressures to move lymph fluid to its destination.
Why is all this important to know? Well, any damage to the lymph system affects flow. When lymph tissues, vessels or nodes are damaged, destroyed, removed or impaired, lymph fluid cannot flow properly! In fact excess lymph fluid will pool in areas causing swelling and pain. This is the beginning of Lymphedema. Depending on the nature, size of the affected area and the time left untreated Lymphedema can spread to affect a whole limb, neck, face or trunk.
While there is no cure for Lymphedema there are manual methods that can be employed to manage the condition and from it getting worse. Treatment options are covered separately in the Complete Decongestive Therapy (CDT) section.
Lymphedema Signs and Symptoms
Lymphedema can affect virtually any part of the body. I have personally seen people suffering from Lymphedema of the face, neck, upper chest, arm and legs during my physical therapy sessions. It usually affects only one limb but in some cases, and especially those with Lipo-Lymphedema, may affect both matching limbs but not always symmetrically. The extent of the Lymphedema will depend on the nature of impacted area and the extensiveness of the node removal or tissue damage.
At first it may not be apparent but it could rapidly expand to encase most the limb, sometime causing swelling that doubles the size of the original limb. Sometimes Lymphedema does not appear until months after damage has been done, as in the case of breast cancer. It may also not appear until Lipedema progresses to the point where the size and amount of Lipedema fat puts too much pressure on the lymphatic vessels and nodes thereby creating impairment in the lymphatic system.
What are the signs and symptoms in the three stages of Lymphedema?

Pre-Stage:
Some have added a pre-stage phase for Lymphedema recognition and treatment. In this pre-stage an overload to the lymphatic system is identified and immediate treatment is started. People respond very well and the Lymphedema is completely reversed.
Stage 1:
- recognition that one limb is larger than the other (tighter fitting clothes, shoes or jewelry)
- feelings of heaviness or tightness
- range of motion difficulty and flexibility
- feelings of tenderness or soreness
- may be warm or red to the touch
- presence of a rash
- pitting edema may occur (pressing on the affected leaves an indentation that slowly returns to normal)
- Stemmer’s sign may be positive or negative
- feelings of embarrassment for others to see a deformation in body
- elevating affected part provides relief and limb should return to normal
- this stage of Lymphedema is reversible
Stage 2:
- feelings of heaviness or tightness
- range of motion difficulty and flexibility (walking impairment if foot is swollen)
- feelings of pain or soreness
- may be warm or red to the touch
- presence of hyperpigmentation (skin discoloration. Mine turned light reddish-purplish in the lower leg area.)
- non-pitting edema occurs (pressing on the affected leaves does not leave an indentation)
- connective tissue fibrosis occurs causing hardened patches of skin and underlying tissues
- Stemmer’s sign may be positive
- feelings of embarrassment for others to see a deformation in body
- feelings of guilt you made this happen (this not your fault! It is the result of an impairment in your body’s function that you did not create.)
- elevating affected area does not bring much relief
- this stage of Lymphedema is irreversible
Stage 3:
- feelings of heaviness in affected area
- fatigue from carrying extra weight in affected area
- restriction in daily activities due to reduced range of motion up to and including immobility
- increased inflammation in tissue resulting in pain
- presence of hyperpigmentation (skin discoloration. Mine turned light reddish-purplish in the lower leg area.)
- pitting edema
- Stemmer’s sign is positive
- skin thickens and becomes lumpy in appearance with an orange peel effect
- lymphostatic elephantiasis occurs ( appearance and touch looks like an elephant’s leg with thick, discolored and large dimpled skin)
- skin flaps or folds may occur
- may develop separate large Lymphedema lobules on limbs
- skin becomes drier and may flakes
- skin cracks or splits open with weeping of lymph fluid (may take time to close and heal)
- significant increase in cellulitis infections which may take weeks, months or years to heal (bacteria infection that settles in affected area causing open sores or wounds. I got mine from untreated strep throat bacteria.)
- increase in fungal infections in the cracks or crevices of skin (proper hygiene is paramount to reduce infections)
- feelings of guilt you made this happen (this not your fault! It is the result of an impairment in your body’s function that you did not create.)
- elevating affected area does not bring relief
- this stage of Lymphedema is irreversible
Note: Some add an additional stage(s) to describe terribly disfigured and diseased limbs affected by Lymphedema. However, most medical organizations consider there to be four stages of Lymphedema with the first stage actually be a pre-stage to Lymphedema and easy to reverse.
Here is a very good Lymphedema resource by Leslyn Keith, Director of Research and Board President for The Lipedema Project and an instructor in lymphedema therapy for Klose Training and Consulting.

Stay tuned for more information on treatment options.
To your improved health!
Resources:
- Medicine.net – Lymphedema
- National Comprehensive Cancer Network – What You Should Know About Lymphedema
- Mayo Clinic – Lymphedema
- BreastCancer.Org – Lymphedema
I think my son (16) is suffering from this. He does a lot of sport and we have had X-rays and an MRI and there is a lot of fluid showing MRI, we are just being referred to plastic surgeon ? not sure why – I assume due to age and general health this may have been disregarded. But following some basic research today this is where I have ended up. We are suggesting compression socks for a few hours a day currently to see if that helps. Based on the above I would think he is at pre-stage Would be grateful for any tips to reduce as he is very conscious of it and feels heavy when doing sport.
Hi Julia!
I am sorry to hear your son is exhibiting symptoms of lymphedema in one or both legs. You may need to see a vascular doctor or a physical therapist that specializes in lymphedema to have his lymphatic system evaluated. He could have a lymphoscintigraphy done to look at the flow of lymph in his legs to look for any abnormalities. It is a specialized test that may be a bit costly but it would see how well his lymph system is performing.
Compression garments help as long as you wear them on a consistent basis. There are different compression levels available in several types of garments. A physical therapist would be best to determine how much compression he would need. Elevating his legs above heart level will also help with pain and flow. Performing manual lymph drainage (MLD) and/or dry brushing will also stimulate lymph flow in the lymph system.
Hope this helps. Best wishes for diagnosis and treatment for your son’s lymphedema!
It is March 2022.
I had the very beginning (Stage 0) in 2018/19.
My knees and ankles were purple/yellow and I could not get up if stooping. I am and was not young then.
Nobody caught it. By Aug 2019, BOTH legs from through to my tip toes were swollen.
Since then I have had sores that weeped, completely different diagnoses, and swelling went down in the entire area. It still is somewhat swollen, including abdomen; but not what it was for almost two years. Now with the swelling I have, the calves are tight and hard. There are some purple small areas. The skin is dry. My right calve a little more swelling than the left. The feet are a little swollen, but not much. Socks at top make big lump of swelling at the top.
Makes no sense to me. My abdomen is swollen, but I am told it IS lymphedema, but not why it is? Maybe I am just fat? Although, I was 93 lbs before all this. Still do not know what constitutes LE in stomach? I have nodes in groin that hurt. They are swollen. Had biopsy on one; OK.
I have other areas where I hurt off and on and probably nodes. So, I am wondering if I might have Lipodema and Lymphedema.
Hi Paula,
I am so sorry that I seem to have missed your message! I understand and sympathize with your pain and swelling problems! Have you seen a physical therapist who specializes in Lipedema and Lymphedema for a diagnosis? Diagnosis is usually made by physical touch and observation. It is quite possible from your description Lymphedema may be involved in addition to the Lipedema. It is difficult to tell if the Lymphedema is a result of Lipedema or another venous condition. You should definitely see a specialist to get a proper diagnosis, which then would dictate the treatment you need to manage your condition.
There are things you can do to help move the excess lymph fluid out of the legs and abdomen areas. These include manual lymph drainage by a professional or self massage using your hands or a dry brush technique. Lymphatic pumps and compression garments will also help contain the swelling providing relief from painful swelling. Some have also found relief in using kinesio tape, vibration plates and low impact exercise and stretching. Have you tried any of these techniques and found success? These would also be necessary to address the softening of possible fibrotic masses (hard areas) in your calves and legs.
Know that you are not alone in your search for answers and help managing your Lipedema and (possible) Lymphedema. I wish you much success in finding the right medical professional to finally diagnosis and begin treatment for your condition!!
Esther
I was just wondering when you say the Pre Stage can be reversed what methods work to do this?
Good question Jess. I must state that I am not a medical practitioner, but rather an educated patient with 35+ years of dealing with Lipo-Lymphedema. Pre-stage treatment depends on where and how the underlying lymphatic impairment has occurred. Many times it is due to radiation treatments, but could be from deep wounds, surgeries or as in my case, lots of Lipedema fat buildup. Assuming a surgical solution is not required for correction, treatment might then entail dietary changes that are targeted at reducing inflammation. You could also incorporate specific exercise(s) aimed at increasing lymph flow in the affected area (working your muscles acts as a pump forcing movement of lymph fluid from node to node). These exercises could incorporate some self-MLD too, ensuring excess lymph fluid does not become trapped in one of your node clusters. If the early pre-stage signs of impaired flow are still present then you might need to move into more aggressive treatment as they do in latter stages of lymphedema. This includes a form of light compression wraps or bandaging and possibly using a pump, which simulates MLD. The trick is knowing you are pre-stage lymphedema and taking prompt action to avoid it progressing!
Hope this helps answer your question.
Thanks for reading my posts and taking the time to work on your health!
Esther
The information provided has been very useful not only as a person who suffers from this condition but also for my studying .
thank you
H King
I am sorry to hear you suffer from lymphedema, but you found the information useful for your needs! Unfortunately, the lymphatic system is not studied in any sort of depth in medical school yet it plays a vital function in our body’s overall health. In fact, the lymphatics are like the yin to the body’s circulatory system yang. You need one system to circulate nutrients to the body and the other system to remove the waste byproducts to keep the system fully functional. Lymphedema needs to be diagnosed and treated as quickly as possible to avoid further complications.
Wishing you much success in your treatment and studies on the lymphatic system!
Esther