Lipedema and Osteoarthritis
Osteoarthritis (OA) is a degenerative joint disease most often affecting the knees, hips, lower back and neck, fingers and big toe. It is the most common chronic joint condition and affects approximately 27 million Americans. (1) Unfortunately, those of us with Lipedema, Lymphedema and Lipo-Lymphedema tend to have an accompanying OA condition as a result of the excessive weight we carry on our body, particularly below the waist and a genetic predisposition to the disease.
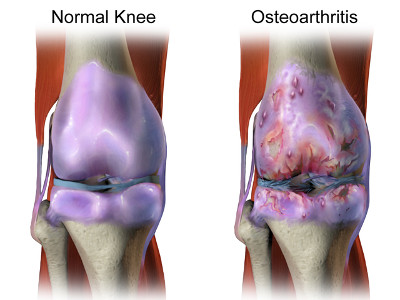 There is a firm rubbery material, called cartilage, that covers the end of each bone that acts like a cushion when two opposing bones move against each other. This helps reduce the friction of bones moving by providing a gliding action that cushions the movement of each bone.
There is a firm rubbery material, called cartilage, that covers the end of each bone that acts like a cushion when two opposing bones move against each other. This helps reduce the friction of bones moving by providing a gliding action that cushions the movement of each bone.
As OA progresses over time, the cartilage wears down or may develop growths, called bone spurs. Pieces of bone or cartilage can also break off and float around the joint area, which can be benign or cause additional pain problems. Inflammation of these affected areas can further damage the cartilage ending up with bone rubbing directly against the opposing bone. This can lead to joint damage and increased pain levels.
Primarily considered a disease of those 65 and over, we are now seeing this show up in younger athletes and those with contributing OA factors. Risk factors include aging, obesity, those with previous joint conditions, weak thigh muscles and genetics.
- One in two adults will develop symptoms of knee OA during their lives.
- One in four adults will development symptoms of hip OA by age 85.
- One in 12 people 60 years or older have hand OA. (1)
What Causes Osteoarthritis?
Science once believed OA was a disease caused by abnormal “wear and tear” on the joints over time. However, a prevailing theory now believes OA is caused by the body’s failed attempt to repair cartilage damage. In healthy cartilage there is a balance between the breakdown and build up of the tissue. In OA this balance is lacking thus leading to complete cartilage breakdown over time.
There are several factors that can contribute to the early onset of OA:
Genetics
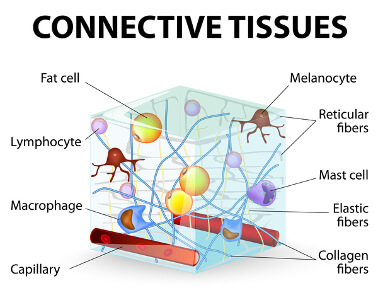 There are people born with various conditions whose bodies for some reason produce weak or faulty collagen, the protein that makes up cartilage. With 80% of the body being made of collagen you can see how faulty collagen could cause extreme problems with our joints, particularly the knees and hips, especially when you add the extra weight to the equation. (See my article on Exercising with Lipedema for more on collagen.) Given those born with this genetic condition, OA could become an issue as early as age 20 or even younger. This includes those of us born with Lipedema and/or other conditions/co-morbidities like Ehlers Danlos Syndrome (EDS).
There are people born with various conditions whose bodies for some reason produce weak or faulty collagen, the protein that makes up cartilage. With 80% of the body being made of collagen you can see how faulty collagen could cause extreme problems with our joints, particularly the knees and hips, especially when you add the extra weight to the equation. (See my article on Exercising with Lipedema for more on collagen.) Given those born with this genetic condition, OA could become an issue as early as age 20 or even younger. This includes those of us born with Lipedema and/or other conditions/co-morbidities like Ehlers Danlos Syndrome (EDS).
Faulty collagen not only affects cartilage but supporting tendons and ligaments as well. While evaluating your joint damage for cartilage damage, don’t forget the support structure that holds the joint together, namely the tendons and ligaments. These could be a source of problems and pain before OA becomes the main problem.
Researchers have found that a gene called FAAH, previously linked to increased pain sensitivity, is higher in people with knee OA than in people who don’t have the disease. (1)
Weight
Here is a topic we know all to well. Carrying around extra weight over time will cause your cartilage to break down faster. Lipedema is an inflammatory disease. Combine that with eating an inflammatory diet (high in sugar and carbohydrates) and you have a recipe for increased damage to all your joints, but particularly your hips and knees where you carry most of your excess weight.
Every pound of excess weight exerts about 4 pounds of extra pressure on the knees. So a person who is 10 pounds overweight has 40 pounds of extra pressure on his knees; if a person is 100 pounds overweight, that is 400 pounds of extra pressure on his knees. “So if you think about all the steps you take in a day, you can see why it would lead to premature damage in weight-bearing joints,” says Dr. Matteson. (2)
For those of us struggling with Lipedema, Lymphedema and Lipo-Lymphedema managing our weight is one of our toughest battles! We know Lipedema is calorie and exercise resistant meaning counting calories and exercising all hours of the day yield little to no weight loss. Therefore, we need to change our food plan to achieve any weight loss and management options coupled with strategic exercises to build good muscle tone.
 Personal note: I am 300 pounds overweight, much of it Lipedema and Lymphedema weight, which means I am putting over 1,200 pounds of extra pressure on my knees. I have severe OA in both knees with bone on bone partially in my right knee. It’s no wonder how I can barely walk from room to room in my home never mind the pain of an extended trip to the doctor’s office!
Personal note: I am 300 pounds overweight, much of it Lipedema and Lymphedema weight, which means I am putting over 1,200 pounds of extra pressure on my knees. I have severe OA in both knees with bone on bone partially in my right knee. It’s no wonder how I can barely walk from room to room in my home never mind the pain of an extended trip to the doctor’s office!
Injury and Overuse
Your body was meant to move. However, repeated sudden or sharp movements, such as the case with athletes, can put unusual stress on the joints, tendons and ligaments causing them to breakdown faster, leading to early OA.
Certain types of jobs involve long periods of time sitting or standing, bending, lifting or other physical movements that are repetitive in nature that lend to cartilage, tendon and ligament breakdown. These “repetitive use” injuries may perhaps start as muscular in nature, but over time without proper care can lead to cartilage breakdown and OA. Be mindful on how you use your muscles and joints as well as the frequency of these movements to help prevent “repetitive use” injuries and OA. Take breaks, alternate standing and sitting, avoid heavy lifting, and mix-up your routine to keep your muscles and joints working optimally.
What are the Symptoms of Osteoarthritis?
Symptoms of OA differ slightly depending which joint(s) is/are affected and the severity of affliction. The most common symptoms are pain and stiffness, especially after long periods of rest or when you wake up. Your joint(s) may also experience swelling after activity or overuse, which is very common in those who suffer with Lipedema and Lymphedema.
- Sore or stiff joints
- Limited range of motion that goes away after movement
- Cracking or popping noise when bending the joint
- Slippage feeling around affected joint(s) (knees in particular)
- Swelling around the joint area
- Pain or aching after activity or overuse
 Pain, swelling and stiffness can make every day tasks difficult to accomplish. These include simple items like grasping a can of food, opening a box, holding something (or someone) in your arms and typing on a keyboard. It can also include walking, climbing stairs, driving a care or lifting objects or even holding a job. Many aspects of your once normal life’s activities may prove challenging if your OA becomes too debilitating.
Pain, swelling and stiffness can make every day tasks difficult to accomplish. These include simple items like grasping a can of food, opening a box, holding something (or someone) in your arms and typing on a keyboard. It can also include walking, climbing stairs, driving a care or lifting objects or even holding a job. Many aspects of your once normal life’s activities may prove challenging if your OA becomes too debilitating.
For some people their symptoms are so severe they can no longer work outside the home and may even have limited abilities getting around within their home. They may need to file for Social Security Disability to help make ends meet. This is what happened to me in 2014 when my severe Lipo-Lymphedema and severe OA (and other comorbidities) prevented me from walking more than about 25 feet before excruciating pain forced me back to bed or my recliner with ice packs and pain medication.
When severe OA occurs it can lead to social isolation. People are either unable or unwilling to deal with the intense pain of OA that they rarely leave their home for social events and lack the ability to entertain in-house. If you have a loved one or know someone with severe OA (and Lipedema) and notice you don’t see them socialize very much, please pay them a visit and offer any services you think might help. They don’t want to be unsocial! It’s the disease and ensuing pain that keeps them prisoner.
Another symptom of OA could be falls. We are at greater risks for falls with weaker muscles in the hips, thighs and legs combined with OA in the hips or knees. People with OA experience as much as 30 percent more falls and have a 20 percent greater risk of fracture than those without OA. (1) This is also true if taking strong pain medications for OA. It could make one dizzy or unbalanced making them more prone to a fall.
Diagnosing Osteoarthritis
Your doctor will collect information about your family history, perform a physical examination and probably order lab tests to look at the affected area(s). They will also look at your personal medical history, medications you are or have taken, reports of the type of pain you’ve been experiencing and if you are experiencing any stiffness or swelling in the affected area(s). They may also order one or more of the following tests:
- Joint aspiration – fluid is drawn out of the affected joint(s) once it is numbed and examined for crystals or deterioration. This test can exclude other medical conditions.
- X-ray – can show evidence of changes to the joint space and how much cartilage still remains in the affected area(s). This is especially useful to see the rate of change when comparing to previous x-rays of the same area.
- MRI – more expensive but a better view of the joint space and structure. It can show a better image of how OA is affecting the joint, cartilage and surrounding support structure.
Treatment Options for Osteoarthritis
There is no cure for OA but there are several management options available to make living with OA more comfortable. These include options for managing pain, stiffness and swelling, and improving joint mobility and flexibility as well as mitigating factors such as weight management and exercise.
Medications
There are several options available from pills to creams to injections to help mitigate OA pain. Options include:
Analgesics – these are pain relievers or pain killers that can be either be purchased over the counter or by a physician’s prescription. They include acetaminophen (Tylenol), opioids or narcotics (Vicodin or Tramadol), and capsaicin creams, lotions or patches.
- NSAIDS (Nonsteroidal anti-inflammatory drugs) – these are the most common type of pain relievers as they also reduce inflammation and can be either be purchased over the counter or by a physician’s prescription. NSAIDS are not meant to be taken long-term as they can cause stomach bleeding and kidney problems for some people. You should also discuss this option with your physician if you are taking blood thinner medications. NSAIDS include ibuprofen, aspirin, naproxen, Advil and Celecoxib.
- Corticosteroids – these are powerful steroid based pain relievers that can be applied topically or via an intra-articular injection (directly into the joint) in your physician’s office. They are available over the counter or by a physician’s prescription. They include hydrocortisone, prednisone and kenalog to name a few.
- Hyaluronic acid – hyaluronic acid is a critical component of the synovial fluid found naturally in the joint which acts as a lubricant when bones move against each other. The U.S. Food and Drug Administration (FDA) has approved these injections for treating OA in the knees with promising results. Other joint injection sites has not been as successful. (3)
 Personal note: I opted for corticosteroid injections (kenalog) every three months to help reduce my excruciating pain in both my knees when common analgesics weren’t strong enough and I couldn’t take most NSAIDS due to allergies. However, since giving up gluten, lowering my carbohydrate intake and moving towards a Ketogenic plan, I have significantly reduced my inflammation levels to the point of not needing the quarterly corticosteroid injections and taking only an opioid as needed for bad pain.
Personal note: I opted for corticosteroid injections (kenalog) every three months to help reduce my excruciating pain in both my knees when common analgesics weren’t strong enough and I couldn’t take most NSAIDS due to allergies. However, since giving up gluten, lowering my carbohydrate intake and moving towards a Ketogenic plan, I have significantly reduced my inflammation levels to the point of not needing the quarterly corticosteroid injections and taking only an opioid as needed for bad pain.
Non-Medication Treatment
 Natural Methods – some people opt for treatments that do not involve long-term medications and the risk of their side effects. Instead they choose to use nutritional supplements, acupuncture or acupressure, massage, relaxation techniques (meditation, yoga, pilates, Reiki, etc.) and hydrotherapy (spa or hot tub), and other treatments for pain relief and management.
Natural Methods – some people opt for treatments that do not involve long-term medications and the risk of their side effects. Instead they choose to use nutritional supplements, acupuncture or acupressure, massage, relaxation techniques (meditation, yoga, pilates, Reiki, etc.) and hydrotherapy (spa or hot tub), and other treatments for pain relief and management.- Physical or Occupational Therapy – some may choose to consult a therapist to actively work on strengthening the joint, learning stretching and moving techniques to improve range of motion, experimenting with hot and cold therapies, pool activities, and investigating other supportive technologies for their joint needs.
- Assistive Devices – these devices can be used to help ease pain and improve function or mobility with most being available at your local medical supply store or through your physician’s or therapist’s office. These include walkers, canes, scooters, braces, orthotics and helper aids such as grippers, bath chairs, and grab bars. Some items are available as generic off the shelf items while others may need to be custom made to your needs by your physician or therapist’s office.
- Surgery – this option may be an alternative for those experiencing a total breakdown of the joint cartilage or supportive space. Consult with your physician to see if this is your best option for regaining functionality or mobility. Hip and knee replacements surgeries are the most common procedures.
Managing Your Osteoarthritis
You have several options for treating your OA once properly diagnosed by your physician as we have discussed above. In addition to medication and non-medication treatments there are things you can do to help you manage your pain and functionality. These include maintaining a healthy weight and getting proper exercise to support the OA in your joint(s).
Healthy Weight Management
 Managing a healthy weight may involve changing your lifestyle, which is something you need to be prepared to do if you want to minimize your pain and regain lost functionality of mobility. I will not tell you which diet plan works best for your body, but there are some simple principles you can apply to help your body heal. The first thing is to eat real whole food that is preferably organic and non-gmo. If it comes from a box it is not real food. I mean lots of fresh vegetables, fruits, meats (unless you’re a vegan) and low carbohydrates, especially those containing mostly sugars. Sugar is an inflammatory agent, which is the very thing you are trying to eliminate and/or control.
Managing a healthy weight may involve changing your lifestyle, which is something you need to be prepared to do if you want to minimize your pain and regain lost functionality of mobility. I will not tell you which diet plan works best for your body, but there are some simple principles you can apply to help your body heal. The first thing is to eat real whole food that is preferably organic and non-gmo. If it comes from a box it is not real food. I mean lots of fresh vegetables, fruits, meats (unless you’re a vegan) and low carbohydrates, especially those containing mostly sugars. Sugar is an inflammatory agent, which is the very thing you are trying to eliminate and/or control.
Once you start eating more healthy any excess weight you’ve been carrying around will soon start to disappear. As I mentioned above getting any excess weight off your joints will help improve your situation. Do your research and figure out which food plan works best for your body and helps you shed any excess weight. The plan needs to be an anti-inflammatory solution so you can heal your body from the inside. Work with your physician or nutritionist to help determine what will work best for you, but do your own research first.
Physical Activity
 One of the best things you can do to help your joint(s) is to move it. You need to carefully move, stretch or use the joint to avoid stiffness and pain. However, be careful not to overdue your exercise. This includes not engaging in an activity too strenuous for your joint or pushing yourself too long in an activity where you overuse the joint(s). Small walks around your neighborhood, the local mall or local school track might be enough to keep the joint(s) properly exercised. However, if this proves too much then walk around your home as much as can to keep the joint(s) in motion.
One of the best things you can do to help your joint(s) is to move it. You need to carefully move, stretch or use the joint to avoid stiffness and pain. However, be careful not to overdue your exercise. This includes not engaging in an activity too strenuous for your joint or pushing yourself too long in an activity where you overuse the joint(s). Small walks around your neighborhood, the local mall or local school track might be enough to keep the joint(s) properly exercised. However, if this proves too much then walk around your home as much as can to keep the joint(s) in motion.
Some find stretching exercises to be the right balance of movement without negatively impacting the joint(s). You can do those at home or find a local class on yoga, pilates or basic stretching to help you with your physical activity. Building up and maintaining supportive muscles around affected joints will help reduce the pain and inflammation giving you greater relief and increased functionality or mobility.
Summary
Osteoarthritis is a degenerative joint disease we generally find comorbid in those with Lipedema, Lymphedema and Lipo-Lymphedema. This is due to the increased size of our limbs and pressure from accumulated adipose fat tissue and lymph fluid in our system. It is also due to the faulty collagen we inherited that creates weak connective tissues, which are found in our cartilage, tendons and ligaments, all the things that comprise our joints. The hips and knees are the most commonly affected OA areas, but can occur in any joint(s) in our body.
Once diagnosed by a physician we can choose treatment options to help manage the pain and inflammation of OA. Depending on the severity and location of the OA we can choose medication and non-medication options. Medication options include topical capcaisin creams, oral pain relievers and anti-inflammatories, or corticosteriod injections. Non-medication alternatives include physical therapies, natural supplements and treatments, assistive devices and surgical joint replacements. Our physician will help monitored our OA condition by determining if treatments are effective and if the OA is progressing towards a total joint breakdown.
Losing excess weight and maintaining a healthy body and weight will help in reducing inflammation and pain in our affected joint(s). This may require a lifestyle change, but isn’t increased functionality or mobility and reduced pain and inflammation worth the change? Do your research and consult with your physician or nutritionist for a food plan that works for your.
Getting enough physical activity to properly work the affected joint(s) area is key to keeping a good range of motion and reducing swelling and stiffness of the joint(s). Just remember not to engage in anything strenuous that puts additional pressure on the joint(s). Instead engage in stretching and low key exercises, such as walking or swimming, building a good support structure in the muscles around the affected joint(s).
Remember to keep a positive attitude and outlook if you’re diagnosed with OA. Studies have shown those with positive attitudes can boost their immune system, which in turn helps the body handle pain. There are many treatment and lifestyle changes you can make to help with reducing pain and inflammation and increasing your functionality and mobility so that you can start to enjoy life again. Partner with your physician to find the best and safest road-map for you in actively managing your OA.
To Your Improved Health!
References:
- (1) Arthritis Foundation – What is Osteoarthritis?
- (2) Arthritis Foundation – How Fat Affects Arthritis
- (3) Arthritis Foundation – Hyaluronic Acid Injections for Osteoarthritis
Resources:
- ResearchGate – Lipedema: A Clinical Challenge-revisited
- US National Library of Medicine – Osteoarthritis
- Arthritis Research and Therapy – Early blockade of joint inflammation with a fatty acid amide hydrolase inhibitor decreases end-stage osteoarthritis pain and peripheral neuropathy in mice
- Arthritis Foundation – Osteoarthritis Blog
Hypermobile Ehlers Danlos Syndrome is common among those with Lipedema. It is also a connective tissue disorder.
Hi Alisha,
Absolutely! I have seen many with Lipedema, especially in the later 3 and 4 stages, present with a co-occurring hypermobility condition. As you have noted they are related connective tissue disorders.
It is both a curse and blessing. On one hand it allows for greater ranges of motion. which is great for donning compression garments. On the other hand it makes your joints lax and prone to subluxation, especially in the knee and hips areas. You must be vigilant in not overextending yourself and cause harm.
Thank you!
Thank you Ester! Finger is worst now. It’s really acting up. I know stress is a part of it. I so appreciate your response that I never got notice on receiving. I saw a massage therapist for lymphedema and did 10 sessions. No luck. I have a splint I have worn but swelling quickly returns. I will try again at night as it may in long run help control it.
I did read a doctor’s case of a flaring event in hands like mine who also didn’t test for RA. He did have all symptoms including pain. Couldn’t grip steering wheel. He didn’t say how long he had had symptoms. He said self diagnosed as seronegitive RA. Remember he is a doc. CRP and ESR were high on blood labs. Conferred with Reumatologist. He did AIG diet and hydroxychloroquine 200 x2 daily. He put all into remission. Found his comment on Micky Trecott’s Autoimmunine Wellness site. Maybe this will help someone. AIG is tough and I have not done it yet. Have Micky’s book. The site is extremely helpful and easy to navigate. Download for free the start up to the diet. Super organized.
I may be going there.
Hi Amie,
Thanks for the update. I am sorry to hear things are getting worse! It is good to do CRP and ESR tests, however, while results indicate inflammation it cannot pinpoint the location nor actual cause of the inflammation. I am not a medical doctor and have limited experience in these type of conditions. It sounds like this could be an autoimmune response since swelling, stiffness and pain are signs of an inflammatory condition. It may not be RA if you don’t have the markers from it. It could be something like dactylitis, which is a sign of an underlying medical condition, quite possibly an autoimmune one. It could also be a venous issue, which a vascular doctor could address, too.
I follow a keto/low carb way of eating to help with all my medical conditions, which has given great relief. I am now looking into how to overlap that with an autoimmune protocol to further help with two of my autoimmune conditions. You can try an AIP plan and see if it helps your condition. However, I would advise you keep your doctor in the loop on any dietary changes so they can advise and monitor your situation for any possible problems.
Wishing you healing success on your journey to identify and treat this condition!!
Esther
Hi, I have OA in my right index finger both joints and it keeps growing and growing and growing. They are huge. My entire finger also is swollen and keeps getting bigger too. Sometimes swelling goes down a bit but goes back up with least bit of sugar, gluten or simple carbs ( organic seed crackers, organic non gluten chips, biodynamic wine, etc). I eat clean but have my moments. I can bend my fat finger with zero pain. My middle finger is showing signs of first joint getting OA. I have seen specialists because of the whole finger swelling and the fact that I can squeeze the fluid to make joints look smaller with a significant change and no pain. I did RA tests and they are neg. Did x-ray and MRI. Two doctors who didn’t spend much time with me said OA. One said on his way out of the exam room that I gripped my pencil too tightly and would be back for a bone fusion. The joint specialist went along with their diagnosis although she was originally intrigued with how large my finger was. She is a brilliant doctor (BARTOV. Morristown, NJ) so I was surprised at her change of direction. Other important fact is I had breast cancer surgery, Sloan Kettering, NYC, on my right side with obviously a lymph removed to check for cancer. Two weeks after surgery I woke up with a golf ball cyst in right arm pit. It was drained but immediately filled again so I had a second surgery. Surgeon is the top at Sloan and said only once in her career did she see something like this. Note: in Europe they do no remove lymph nodes to test for cancer and instead use other methods. I am guessing this was a clogged lymph node. What do you think? My finger, about 8 months after surgery had a little bump on the index finger’s first joint. This, over the next 3 years, just grew. By March 2020 it was clearly a huge disfigured joint and at this time the top half of my finger (above second joint) starred swelling. My nail has been stretched flatter and a side view shows even my finger pad is so swollen. Sometimes red or red/purple. 9 months later my second joint started swelling and so did the rest of my finger. I see no skin wrinkles on my first joint. At times I don’t see the skin wrinkles on my second joint and I have very fleshy skin there. Mind you I can bend both joints no problem. The fluid gets in the way of at first joint but after a minutes of applying pressure to make it bend more it looks better. No pain.
I am perplexed as this seems to be an odd case as I find nothing like this on the internet. I am wondering if my lymph node(s) are clogged and that is why there is swelling? Could it be that the swelling or fluid came first by seeping into my joint which is the farthest point down my arm then caused the OA to start by disfiguring the joint? The more the lymph is clogged the more the fluid gets trapped in my finger. I mentioned my middle finger first joint is getting a bump and will add my ring finger is too. My left hand is great. I am also in good health and have fought Lyme after 6 years of finally getting the correct diagnosis. After antiobiotics got me so sick I found an integrative doctor who is nearby and well versed in the treatment modalities. Lucky to have this put into remission after three years. I have a determined spirit and know this finger issue can be bested as well.
I am hoping due to your knowledge of both lymph and OA that you may connect dots that my doctors could not. If you see a connection here could you guide me on a protocal and they type of doctor to see. If you know a doctor in my area I would be grateful for a recommendation. Thank you for reading through this message too.
My best, Amie
Hi Amie,
I am so sorry you are suffering with this problem in your hands and fingers! However, I am really glad to see your fighting spirit and your need to find an answer to this perplexing problem! I am not a doctor and cannot advise you in any manner; I can only make suggestions for people to help you or things to consider exploring. Combinations of conditions, such as your breast cancer, Lyme disease, OA, possible leaky gut or immunity issues, could all be a factor in the swelling of your hands and fingers. Have you seen a physical therapist who might be evaluate you, specifically one trained in Lymphedema? Is it possible you have ganglion cysts in your hand or between your joints that could be flaring causing you swelling or pain?
You are definitely doing a great job severely restricting the sugars, reducing your carbs and limiting gluten! Those are all sources of inflammation that raise swelling and pain, especially in the joints. Does massaging the fingers help keep the swelling down? Have you tried any type of hand and finger compression garments to keep the swelling under control? I know they work wonderfully for my Lymphedema and OA in my legs.
These are the immediate things that come to mind to try and help your situation. I sincerely hope you identify the cause and work to eliminate or manage the problem going forward! Wishing you improved health!!
Esther
This article brought me to tears, I felt very alone and alienated dealing with the impact of significantly reduced mobility. I have severe bone on bone arthritis in both knees. My hips, fingers and S.I. joints are also affected. I worked in a primary care and multi specialty care medical clinic for 30 years. In the last ten years my symptoms have increased and I was able to somewhat manage them with NSAIDs until I was Diagnosed with Atrial Fibrillation and started on blood thinners thus requiring me to discontinue NSAIDs. Within two weeks of discontinuing them my SI joint pain became unbearable and though I had a sedentary job, I was no longer able to sit in an upright position for more than two hours due to severe pain. Over the years I have consulted with many of the specialists whom I worked with on a daily basis. Despite the fact that I explained that I didn’t loose weight below my waist and in my upper arms no matter how much I deprived myself of food or how much I exercised, the recommendation was always eat less and exercise more.
It was just recently that I learned about Lipedema and though I do not have an official diagnosis, I am quite certain I have it. I also believe my daughter has it and I wish she could get diagnosed so she can make decisions that will minimize her symptoms and help her not have the OA comorbidity. I have lost faith in the specialists that I worked with and consulted as I feel like they failed me and so many others by not being aware of Lipedema! As of yet, I have not been successful with finding a physician in Washington state who will evaluate us.
Hi Madison,
My heart just breaks knowing you are suffering not only with possible Lipedema but OA as well! I, too, have a bone on bone situation in my knees and my SI joint makes it uncomfortable to sit for any length of time. Connective tissue disorders mean we have looser joints, deteriorating cartilage, leaky cell walls, often digestive issues and may even have complications with hypermobility. Unfortunately, training on fat disorders. lymphatic conditions, and other connective tissue disease is not widely taught in Western medicine, so doctors are at a disadvantage trying to diagnose then treat these diseases. That is why we must advocate for ourselves and others so we can raise awareness in the medical community thereby getting the required treatment for these conditions. Here is a place you can try and find a doctor who can diagnose you and your daughter – https://lipedemaproject.org/lipedema-lipoedema-lipodem-provider-directory/ .
I used to take NSAIDS and cortisone injections in both knees for high levels of pain in my joints. I had to discontinue NSAIDS due to allergies and stomach issues. I also found the effects of cortisone injections only lasted 6-8 weeks before the intense pain returned. What I have discovered that works better than medications is changing my way of eating. I no longer rely on medications for pain by eliminating grains (I have Celiac disease) and reducing my carbohydrate intake to under 50g per day. I have adopted a low carb / keto eating way of life and I can honestly say the significant reduction in inflammation and pain has been astounding! You can also shed quite a bit of weight (from normal fat, not Lipedema fat), which has helped me regain some of my mobility. Perhaps this is an avenue you can pursue and see if it can help with both the Lipedema and OA management! You can read more about it on my page – https://morethanfat.com/what-is-lipedema/lipedema-inflammation-and-keto-way-of-eating .
Wishing you much success on your health journey! Please let me know if I can be of further assistance.
Hi I have lipodema and osteo arthritis in a previously injured knee. I have been able to keep my weight in check but still I am 20 plus pounds overweight since I was 12 yrs. old. I have had some connective tissue problems with my fascia and now do fascia blasting to keep my mobility range. It really has helped.
Oh no, Deb, I must have missed your comment when I was in the hospital. Yes, I have heard people have had great success in fascia blasting, too. I must admit I haven’t done this yet, but it is on my list to try. I have found that greatly reducing my carbs, whether doing a low carb or keto plan, has significantly reduced my pain and inflammation in both my knees! I can now manage the pain without regular cortisone injections or opioid treatments. Any weight you can get off the knees will help the OA and maintain mobility.
Thank you letting me/us know how fascia blasting has helped you with your OA! May you have continued good health!
Esther